What to Expect After Disc Replacement Surgery of the Neck
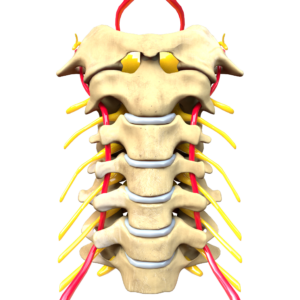
The aftermath of disc replacement surgery in the neck can be a complex process, encompassing not only physical recovery but also emotional and psychological adjustments. Patients may be faced with temporary discomfort, limited mobility, and a range of other symptoms. However, with a solid understanding of post-operative care, effective pain management strategies, and the potential lifestyle adjustments needed, one can navigate this journey more efficiently. We invite you to explore this subject further, as we investigate the essential aspects of what lies ahead after such a surgery. Understanding Disc Replacement Surgery Delving into the intricacies of disc replacement surgery, it’s imperative to understand that this procedure entails the removal and replacement of a damaged cervical disc with an artificial one, a medical intervention designed to alleviate neck pain and restore mobility. The surgery involves a small incision in the front of the neck, through which the damaged disc is removed and replaced with a prosthetic disc. It’s a sophisticated procedure that requires precision and expertise, often performed under general anesthesia. Despite its efficacy, disc replacement surgery is not devoid of surgical risks. These include potential damage to surrounding blood vessels, nerves, or the spinal cord, infection, graft rejection, or failure of the artificial disc. Additionally, there’s a risk of persistent pain or the inability to achieve desired mobility post-surgery. Alternative treatments exist for individuals who may be ineligible for surgery or prefer a non-surgical approach. These include physical therapy, pain medications, corticosteroid injections, or lifestyle modifications. However, these alternatives may not provide the same degree of relief as surgery and may not be as effective for severe disc damage. Hence, a thorough discussion with a healthcare provider is essential to understand the best treatment option. Immediate Post-Operative Experience The journey towards recovery begins immediately following the disc replacement surgery, encompassing a range of post-operative experiences that vary in severity and duration based on individual circumstances. A well-informed patient can manage these experiences better by understanding what to expect and how to handle them. Here are some immediate post-operative experiences: Pain and discomfort: It is common to experience neck pain and general discomfort after the anesthesia wears off. Pain management is typically done through medication and should be discussed with the surgeon or nurse. Surgical anxiety: Patients may experience anxiety about their recovery. It is important to address these concerns with healthcare professionals who can provide reassurance and accurate information. Physical limitations: Initial mobility might be limited, and patients may require assistance for routine tasks. Emotional support: The significance of emotional support cannot be underestimated. Family and friends can offer comfort and assistance, which can accelerate the healing process. These experiences are part of the recovery process and are typically temporary. Keep in mind that everyone’s recovery journey is unique; hence, experiences will vary. Open communication with healthcare professionals will help manage expectations and enhance the healing process. Hospital Stay Duration The duration of a hospital stay following neck disc replacement surgery is dependent upon a number of variables, including individual




