In the domain of medical science, particularly concerning spinal health, there exists a multitude of neck surgery types. These range from cervical discectomy and fusion surgery to more complex procedures like cervical corpectomy and laminoplasty. Each surgery carries its own set of objectives, methodologies, and potential risks. As we broach this intricate topic, it is crucial to contemplate the breadth of these procedures and their respective roles in patient recovery, thereby illuminating the vast landscape of options available in neck surgery.
Understanding Neck Surgery
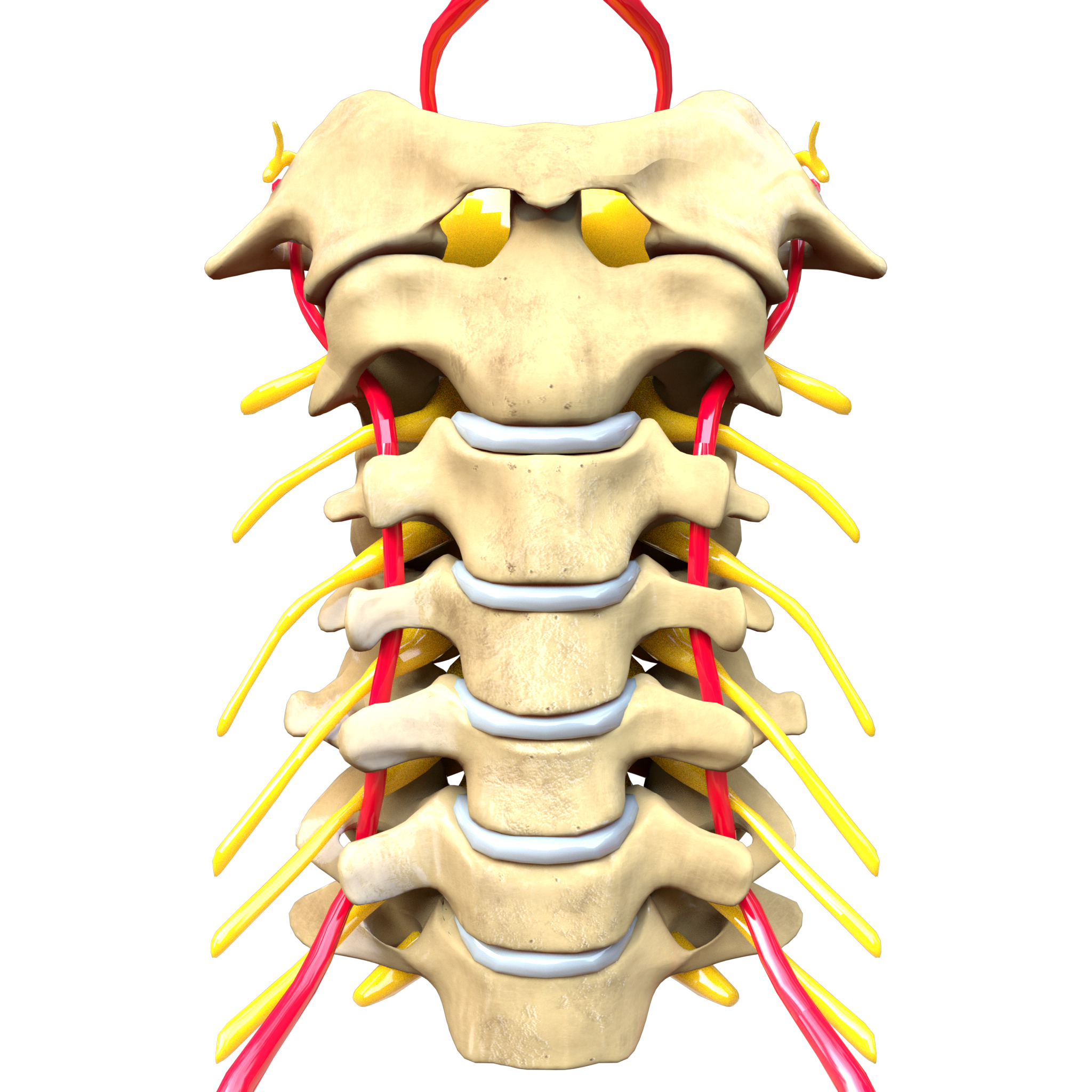
To fully understand neck surgery, it’s important to explore the intricate anatomy of the cervical region and the diverse range of procedures that can be executed to alleviate various conditions. The cervical region is a complex network of nerves, muscles, and vertebrae, the understanding of which lays the foundation for grasping surgical interventions.
Neck surgery is often a last resort after the exploration of neck surgery alternatives. These alternatives include physical therapy, pain management through medication, or minimally invasive procedures such as injections or nerve blocks. The decision to proceed to surgery is made after a thorough evaluation of the patient’s condition, including the severity and duration of symptoms, and the patient’s overall health status.
Pre-surgical preparations play a critical role in the success of the procedure. These preparations involve a thorough medical evaluation, including imaging studies to pinpoint the exact source of the problem. Patients may also be required to cease certain medications, and in some cases, improve their physical condition to better withstand the rigors of surgery.
Ultimately, the goal of neck surgery, like any surgical intervention, is to alleviate symptoms, improve quality of life, and prevent further deterioration.
Cervical Discectomy: An Overview
One of the more commonly executed types of neck surgery is cervical discectomy, a procedure specifically designed to address issues related to herniated or degenerative discs in the cervical region of the spine. This surgical intervention involves the removal of the offending disc to alleviate pressure on the nerve roots or spinal cord, which can cause severe pain and other neurological symptoms.
The process of cervical discectomy can be categorized into several key stages:
- Patient preparation: Pre-surgical evaluations and discussions about patient experiences are essential for determining the suitability and potential benefits of the surgery.
- Surgical approach: The surgeon accesses the cervical spine either from the front (anterior discectomy) or the back (posterior discectomy).
- Disc removal: The herniated or degenerated disc is carefully removed to relieve pressure on the spinal nerves.
- Recovery: Post-operative care typically involves physical therapy and pain management strategies.
While discectomy is often successful in alleviating symptoms, it’s not the only solution available. Discectomy alternatives such as non-surgical treatments, minimally invasive procedures, or different types of surgery may also be considered depending on the patient’s condition, preferences, and the surgeon’s judgment.
Details on Cervical Fusion Surgery
Cervical fusion surgery, a widespread form of neck surgery, requires a thorough exploration. It is relevant to discuss not only the procedure itself but also the inherent risks and potential complications that come with this surgical intervention. Additionally, the post-surgery recovery process, which plays a crucial role in patient outcomes, deserves detailed analysis.
Understanding Cervical Fusion Surgery
Exploring the complexities of cervical fusion surgery, it is important to recognize that this procedure involves the joining, or fusion, of two or more cervical vertebrae in an effort to stabilize the spine and alleviate pain. A detailed understanding of this surgical approach requires an examination of cervical fusion alternatives and an assessment of fusion surgery costs.
- Cervical Fusion Alternatives: These could include non-surgical treatments such as physical therapy, pain medication, or therapeutic injections.
- Fusion Surgery Costs: These can vary widely depending on factors such as location, surgeon experience, and whether or not insurance covers the procedure.
- Surgical Procedure: The surgeon removes the disc between two vertebrae, then fuses the bones together with a graft.
- Recovery: Post-operative care involves rest, physical therapy, and careful monitoring of the healing process.
Risks and Complications
While the efficacy of cervical fusion surgery in providing stability and pain relief is well-documented, it is equally important to critically examine the potential risks and complications associated with this surgical procedure. Anesthesia impact, for instance, could lead to adverse reactions such as nausea, vomiting, or more serious cardiovascular complications. Despite the surgeon’s precision, there is also the possibility of damage to the surrounding tissues, nerves, or the spinal cord. Infection, bleeding, and non-union of the fused vertebrae are other potential risks. Alternatively, therapies like physical therapy or spinal injections might serve as effective, less invasive options. These options, however, may not provide the same level of stability or long-term relief as surgery. Therefore, evaluating the potential risks against the benefits is essential in deciding the best treatment route.
Post-Surgery Recovery Process
After a cervical fusion surgery, patients begin a recovery process that is multifaceted and can be divided into distinct phases, each with specific objectives and milestones to gauge progress. This process typically involves:
- Immediate post-operative care: The focus here is on pain management strategies, ensuring patient comfort and monitoring for any immediate post-operative complications.
- Physical therapy: Commences once the patient has stabilized. The benefits of physical therapy are numerous, including improving mobility, strength, and overall function.
- Long-term management: Involves continuing physical therapy, maintaining a healthy lifestyle, and monitoring for any late complications.
- Regular follow-ups: These are essential to assess the progress of recovery and make necessary adjustments to the treatment plan.
This holistic approach ensures optimal recovery and rehabilitation post cervical fusion surgery.
Unpacking Cervical Laminectomy
Cervical laminectomy, a surgical procedure aimed at relieving neck pain and neurological symptoms, requires careful analysis due to its intricate nature. This discussion will encompass the meticulous procedure, along with potential risks and complications that may arise during or post-surgery. Additionally, emphasis will be placed on an integral part of the healing process: post-surgery care and recovery.
Understanding Cervical Laminectomy Procedure
In the domain of neck surgery, one often encounters the intricate procedure known as cervical laminectomy, which involves the removal of a portion of the vertebral bone called the lamina to alleviate pressure on the spinal cord or nerves. Understanding the cervical spine anatomy is essential to comprehend the procedure.
- Laminectomy is usually a last resort, undertaken when laminectomy alternatives like physiotherapy or medication have failed.
- The surgeon accesses the cervical spine through an incision in the back of the neck.
- The lamina is carefully removed, freeing the spinal cord or nerves from compression.
- After the procedure, the surgeon closes the incision, and recovery begins.
Each step requires meticulous planning and execution, underlining the complexity of this surgical intervention.
Potential Risks and Complications
In addition, the execution of a cervical laminectomy procedure is a meticulous process, it is equally important to contemplate the possible risks and complications that could arise post-surgery. These may include infection, nerve damage, and spinal fluid leak, among others. Risk management techniques and complication prevention strategies such as rigorous pre-operative planning, sterile surgical environment, and precision during surgery can mitigate these risks. Additionally, the surgeon’s skill and experience play a pivotal role in reducing complications. A deep understanding of the patient’s health status, careful selection of anesthesia, and diligent intraoperative monitoring are also key to ensuring a successful outcome. Despite these precautions, it is essential for patients to comprehend that every surgical procedure carries inherent risks.
Post-Surgery Care and Recovery
Following a cervical laminectomy, the postoperative period demands meticulous care and a structured recovery plan to guarantee maximum healing and to minimize potential complications. The recovery process typically involves various pain management techniques and a series of rehabilitation exercises.
The primary components of post-surgery care and recovery include:
- Pain management: Techniques such as medication, nerve blocks, and alternative therapies can be employed to manage postoperative pain effectively.
- Rehabilitation exercises: A structured regimen of exercises under the guidance of a physical therapist aids in regaining strength and flexibility.
- Wound care: Regular cleaning and monitoring of the surgical site can prevent infection.
- Regular follow-ups: Routine check-ups with the surgeon are necessary to track progress and address any arising issues.
Each component is critical for a successful recovery and return to daily activities.

Dive Into Anterior Cervical Discectomy
Anterior Cervical Discectomy is a surgical procedure that involves the removal of an intervertebral disc or a portion of this disc from the neck area, specifically the cervical spine, to alleviate spinal cord or nerve root pressure and address associated symptoms. This procedure is most commonly performed when patients suffer from symptoms related to cervical disc herniation, such as severe neck pain, numbness, weakness, or paralysis.
Discectomy success rates are generally high, with a significant proportion of patients reporting relief from painful symptoms post-surgery. Studies have indicated success rates ranging from 73% to 83%. The exact rate can vary depending on factors such as the patient’s overall health, the specific nature of the disc problem, and the surgeon’s expertise.
It is essential to note that surgery is typically considered the last resort after non-surgical alternatives have been explored. Non-surgical interventions may include physical therapy, medication, chiropractic care, and lifestyle changes such as weight reduction and cessation of smoking. The choice between surgical and non-surgical treatment should be made carefully, considering the severity of the symptoms, the patient’s overall health, and the potential risks and benefits of each approach.
Posterior Cervical Laminotomy Explained
Posterior Cervical Laminotomy is a surgical procedure aimed at relieving pressure on the spinal cord or nerve roots in the neck, typically caused by a herniated disc or spinal stenosis. The procedure and recovery process involve removing a portion of the lamina to alleviate the pressure, followed by a post-operative period of careful monitoring and rehabilitation. However, like all surgical interventions, it carries potential risks and complications, which need to be thoroughly evaluated against its potential benefits.
Understanding Posterior Cervical Laminotomy
In the field of neck surgery, Posterior Cervical Laminotomy emerges as a sophisticated procedure aimed at relieving pressure on the spinal nerves in the neck region. Its effectiveness has been duly proven, yet it stands as one of the many alternative treatments available for cervical spinal conditions.
To further grasp the concept, the following elements are key:
- Laminotomy Effectiveness: This surgery has shown substantial effectiveness in alleviating symptoms related to nerve compression, such as pain, numbness, and weakness.
- Alternative Treatments: Other options include physical therapy, medications, and less invasive procedures like cervical epidural injections.
- Procedure Specifics: The surgery involves a small incision in the neck, removal of a portion of the vertebrae (lamina), and sometimes a discectomy.
- Potential Risks: As with any surgical procedure, risks may include infection, nerve damage, and spinal fluid leaks.
Procedure and Recovery Process
Delving deeper into the specifics of Posterior Cervical Laminotomy, the procedure and subsequent recovery process are essential to understanding the effectiveness and implications of this surgical intervention. Surgeons performing this operation remove a portion of the vertebrae to relieve pressure on the spinal nerves, often presented as a surgical alternative when conservative pain management strategies have been ineffective.
Post-surgery, patients may experience immediate relief, but full recovery often takes weeks to months. Pain management post-operation involves controlled medication and physical therapy. The rehabilitation program focuses on strengthening neck muscles and improving flexibility. During this period, patients are advised to avoid strenuous activity and follow a progressive exercise routine. The recovery timeline and success rate of this intervention underscore its role among neck surgery options.
Potential Risks and Complications
While the recovery process of a Posterior Cervical Laminotomy generally yields positive outcomes, it is equally important to take into account the potential risks and complications associated with this surgical procedure.
Some of the risks inherent to this type of neck surgery include:
- Anesthesia risks: These encompass a spectrum of complications such as allergic reactions, respiratory difficulties, and cardiovascular issues.
- Postoperative infections: Despite stringent sterilization protocols, there’s a small chance of infection at the incision site or internally.
- Nerve damage: Although rare, there’s the possibility of nerve damage which could result in pain, numbness, or weakness.
- Dural tear: An unintentional tear of the dural sac enclosing the spinal cord could lead to cerebrospinal fluid leakage.
Understanding these risks enables informed decision-making for both the patient and surgeon.
Insight on Cervical Foraminotomy
Cervical Foraminotomy, a noteworthy procedure in the field of neck surgeries, involves the careful removal or resizing of parts of the cervical spine in order to alleviate nerve root pressure. This surgical intervention is primarily utilized to treat cervical radiculopathy, a condition characterized by nerve root compression leading to pain, weakness, or numbness in the neck, shoulder, and arm regions.
Foraminotomy success rates are markedly high, with about 80-90% of patients experiencing substantial relief in symptoms post-surgery. The effectiveness of this procedure is amplified when accurately diagnosing the source of nerve root compression, followed by meticulous surgical execution.
However, like any surgical intervention, Cervical Foraminotomy is not devoid of risks. Hence, alternative treatments to foraminotomy are often explored before resorting to this invasive procedure. Non-surgical treatment methods such as physical therapy, medication management, and epidural steroid injections serve as potential alternatives. These non-invasive treatments aim to reduce inflammation and pain, improve functional mobility, and foster the natural healing process.
Ultimately, the decision between surgical and non-surgical treatments should be based on individual patient condition, including the severity of symptoms, overall health status, and personal preference.
What Is Posterior Cervical Fusion?
Posterior Cervical Fusion, another significant procedure in the domain of neck surgeries, involves the fusing of two or more cervical vertebrae in the neck to improve stability, correct a deformity, or reduce pain caused by abnormal motion. This technique is often employed when other less invasive methods have failed to provide sufficient relief.
The surgery involves making an incision at the back of the neck, exposing the cervical spine, followed by the careful placement of bone grafts between the affected vertebrae. Subsequently, screws and rods are used to hold the vertebrae together while the bone graft heals and fuses the vertebrae.
The posterior cervical fusion surgery offers several benefits:
* Stabilizes the neck, eliminating abnormal motion
* Provides substantial relief from pain and discomfort
* Corrects spinal deformities
* Prevents further degeneration of spinal structures
The post-surgery period is critical, and pain management post surgery is an integral part of recovery. Fusion alternatives are considered when there is a high risk of non-fusion or pseudoarthrosis, and these may include the use of bone growth stimulators or additional surgical procedures. Each patient scenario is unique, and the surgeon will decide the best course of action based on individual circumstances.
Cervical Disc Replacement Surgery
In contrast to the fusion-based procedures, another prominent intervention in neck surgeries is the Cervical Disc Replacement Surgery, a technique designed to replace a damaged cervical disc with a prosthetic one. This surgery aims to alleviate symptoms like pain, numbness, or weakness resulting from a degenerative or herniated disc.
The procedure involves the removal of the affected disc and its replacement with an artificial one, which mimics the natural disc’s structure and function. This offers an important advantage in preserving the neck’s mobility and flexibility, unlike fusion surgeries that can restrict movement.
The longevity of the artificial disc is an important aspect to consider. Advanced medical engineering has resulted in artificial discs that are durable and capable of withstanding daily wear and tear. They are designed to last for many years, often outliving the patient’s lifespan. However, further research is needed to establish long-term outcomes definitively.
Insurance coverage intricacies for this procedure can vary significantly. While most insurers recognize the surgery as a viable treatment option for specific conditions, the coverage details can differ. Patients should consult with their insurance provider to understand the extent of coverage for Cervical Disc Replacement Surgery.
Cervical Corpectomy: The Basics
While there are various surgical options for treating neck-related ailments, one highly specialized procedure that merits consideration is cervical corpectomy, a technique primarily aimed at relieving pressure on the spinal cord and nerves. Originating from the Latin ‘corpus’ (body) and the Greek ‘ektome’ (removal), corpectomy involves the removal of a portion or all of a vertebral body to decompress the spinal cord and nerves.
Corpectomy history dates back to the 1950s, and since then, the procedure has greatly evolved due to advancements in surgical techniques and technologies. Despite its historical effectiveness, corpectomy alternatives have emerged, providing patients with a broader range of treatment options.
Corpectomy’s key characteristics include:
- A surgical approach through the front (anterior) of the neck
- Removal of one or more vertebral bodies
- Use of a bone graft or a metal cage to maintain spinal stability
- Potential fusion of adjacent vertebrae
Each of these elements contributes to the overall objective of relieving spinal cord and nerve pressure. While corpectomy can be an effective solution for certain patients, it’s important to remember that it, like all surgical procedures, carries potential risks and complications. Discussions about surgical options should always involve a thorough evaluation of the patient’s unique condition and needs.
Cervical Laminoplasty: A Deep Dive
Shifting our focus to another important surgical procedure, cervical laminoplasty, it is essential to examine the intricate details and technical aspects of this operation, designed primarily to alleviate spinal cord compression. This procedure involves reshaping or repositioning bone to create more space for the spinal nerves or spinal cord. The surgeon cuts the lamina (part of the vertebra) on one side and swings it open like a door. This is done to relieve pressure on the spinal cord and give it more room.
The laminoplasty procedure cost can vary, contingent upon the hospital, the surgeon’s experience, and the patient’s overall health condition. However, it’s generally an expensive procedure due to its complexity and the specialized equipment used.
Post-operation, the recovery diet after laminoplasty plays an important role in the healing process. It should be rich in protein, vitamins, and minerals to aid tissue repair and improve the body’s immune response. Hydration is equally important. Foods high in fiber are recommended to counter the effects of analgesics and anesthetics, which often cause constipation.
Posterior Neck Surgery: An Exploration
Posterior neck surgery, an intricate and specialized procedure, involves operating on the back of the neck to alleviate pain or correct anomalies in the cervical spine. Several posterior approach benefits make this procedure a viable option for many patients. These benefits include direct access to the problematic area, less disruption of the neck muscles, and improved post-operative outcomes.
Despite these advantages, posterior neck surgery should be considered only after exhausting non-surgical alternatives. Non-surgical methods can effectively manage various neck conditions, and they often come with fewer risks than surgical interventions.
The following points provide a visual representation of key ideas:
- Posterior neck surgery offers direct access to the problem area, enabling surgeons to operate with precision.
- There is less disruption of neck muscles in the posterior approach, reducing post-operative pain and facilitating faster recovery.
- Non-surgical alternatives should always precede surgical intervention. These may include physical therapy, medications, and lifestyle modifications.
- Despite its benefits, posterior neck surgery comes with potential risks, such as infection and nerve damage, which must be discussed thoroughly with the patient.
Frequently Asked Questions
What Are the Potential Risks and Complications of Neck Surgery?
Potential risks and complications of neck surgery include anesthesia risks such as allergic reactions or respiratory complications, and surgical site infections that can lead to prolonged healing, scarring, or in severe cases, sepsis.
How Long Does Recovery Typically Take After Neck Surgery?
Recovery time after neck surgery varies based on the procedure, individual health, post-surgery nutrition, and adherence to rehabilitation exercises. Generally, it ranges from several weeks to a few months for full recovery.
Are There Non-Surgical Alternatives to Treat Neck Conditions?
Yes, non-surgical alternatives for treating neck conditions exist. Chiropractic benefits include pain relief and improved mobility. Acupuncture is also effective, reducing inflammation and enhancing blood flow, thereby alleviating symptoms associated with various neck conditions.
How Effective Is Neck Surgery in Relieving Symptoms?
The effectiveness of neck surgery in symptom relief varies based on the individual case. A thorough surgery cost analysis and post-surgery physiotherapy plan can greatly contribute to the success of the procedure and symptom alleviation.
What Lifestyle Changes May Be Necessary After Undergoing Neck Surgery?
After neck surgery, appropriate lifestyle modifications are essential. These may involve post-surgery nutrition adjustments to facilitate recovery and recognizing exercise limitations to prevent strain, while gradually strengthening neck muscles under professional guidance.