The immobilization of the neck during surgical procedures is an essential aspect that greatly impacts the surgery’s overall success. Specialized frames or positioning devices are commonly used to guarantee the neck’s stability, which subsequently allows surgeons to perform with utmost precision while reducing the risk of potential complications. This practice also aids in maintaining the alignment of the cervical spine for ideal surgical access. However, one might wonder, what specific factors influence the choice of these devices, and how do they ensure patient comfort and safety throughout the process?
Understanding Neck Anatomy
How does the intricate architecture of the human neck contribute to its function and mobility? The answer lies in the complex interplay of the musculature and the vertebral column structure. The neck, or cervical region, is a marvel of biomechanical engineering, designed to provide support, flexibility, and protection for essential neurovascular structures.
In terms of the Neck Musculature Overview, there are two main groups: the superficial and the deep muscles. The superficial muscles, such as the sternocleidomastoid and the trapezius, are primarily involved in gross movements and maintaining postural stability. The deep muscles, including the scalenes and the longus colli, contribute to fine motor control, allowing for movements such as flexion, extension, and rotation.
The Vertebral Column Structure complements the musculature to provide a flexible yet sturdy framework. The cervical spine consists of seven vertebrae, uniquely shaped to enable a wide range of motion. The intervertebral discs act as shock absorbers, while the facet joints facilitate movement. The vertebral foramina, formed by the vertebral arch and body, house and protect the spinal cord.
Understanding this intricate architecture can provide valuable insights into the challenges and considerations of neck surgery.
The Preoperative Assessment
The thorough assessment, an essential step prior to neck surgery, primarily focuses on two key areas: the patient’s overall health and the potential risks associated with the operation. A detailed evaluation of the patient’s health not only includes a meticulous review of their medical history, but also a thorough physical examination to detect any conditions that may complicate the procedure. Risk determination, on the other hand, involves an analysis of potential surgical complications, factoring in the patient’s unique health profile and the specific surgical technique to be employed.
Assessing Patient’s Health
Before neck surgery, a thorough preoperative evaluation of the patient’s overall health is essential in optimizing surgical outcomes and minimizing potential risks. This process involves a detailed analysis of the patient’s health history relevance, including prior medical conditions, surgeries, and medications, which could influence surgical planning and postoperative recovery. As part of this assessment, physicians should also conduct a lifestyle impact assessment. This includes evaluating the patient’s current diet, physical activity levels, smoking, and alcohol consumption habits. These factors can have a substantial impact on the patient’s immune response, wound healing, and overall recovery. A thorough preoperative health assessment allows for the identification of potential medical issues that may require management before surgery and not just the neck’s positioning during the operation.
Determining Surgery Risks
In the preoperative assessment phase, a systematic approach is employed to identify potential surgery risks, including inherent patient-related factors, the severity of the neck condition, and the complexity of the proposed surgical procedure. A thorough evaluation of the patient’s overall health, previous medical history, and current physical status is conducted. Risk mitigation strategies are developed based on the assessment results, aiming to minimize possible complications and increase surgical success rates. These strategies may include optimizing the patient’s overall health before surgery, selecting the most appropriate surgical technique, and planning for potential intraoperative challenges. The assessment also provides insights into postoperative care requirements, enabling the healthcare team to prepare for possible postoperative complications.
Importance of Neck Immobilization
Recognizing the essential role of neck immobilization during surgery underscores its significance in reducing the risk of potential complications and ensuring ideal patient outcomes. Immobilization techniques are pivotal in maintaining spinal alignment, preventing neural damage, and facilitating an adequate surgical field. The use of rigid cervical collars, halo vests, or Gardner-Wells tongs are some of the common methods employed to achieve this.
The choice of technique largely depends on the type of surgery, anatomical considerations, and the patient’s overall health status. Proper immobilization safeguards critical structures in the neck, such as the spinal cord, nerves, and blood vessels, from inadvertent injury.
Recovery implications are also closely tied to immobilization. A well-immobilized neck can facilitate faster healing, prevent post-operative complications, and promote a smoother rehabilitation process. Unwanted movements during recovery could lead to wound dehiscence, delayed healing, or even neurological complications. Postoperative immobilization strategies, such as the use of neck braces or supports, are also essential.
Common Neck Surgery Procedures
In the context of neck surgery, there are a number of common procedures that are frequently employed by surgeons. These include, but are not limited to, various types of cervical spine surgeries, anterior cervical discectomy, and posterior cervical fusion. Each of these procedures has its own set of specific indications and techniques, which will be discussed in the following sections.
Cervical Spine Surgery Types
Various types of cervical spine surgery, often referred to as neck surgery procedures, are meticulously designed to address specific structural problems in the cervical spine. These procedures have evolved greatly, thanks to cervical surgery innovations. For example, Cervical Laminectomy and Laminoplasty surgeries eliminate pressure on the spinal cord by removing the lamina, thereby enhancing spine health maintenance.
Cervical Foraminotomy, another procedure, focuses on relieving pressure on nerve roots. The surgical removal of a herniated or degenerated disc, known as Cervical Discectomy, is another popular method. These surgeries, combined with spinal fusions, can stabilize the spine and reduce pain.
It is important to note that each surgery type has its unique benefits and risks, therefore, the selection of a particular procedure depends on the patient’s condition and the surgeon’s assessment.
Anterior Cervical Discectomy
Shifting our focus to a frequently performed neck surgery, Anterior Cervical Discectomy stands out as a key procedure in alleviating neck pain and related symptoms. This surgery involves removing an intervertebral disc or part of it, which may be causing pain due to herniation or degeneration.
- The discectomy recovery timeline varies from patient to patient, generally spanning between 4 to 6 weeks.
- Pain management is essential during the recovery period and typically involves prescribed medications.
- Physical therapy is often recommended to restore strength and flexibility.
- Alternative treatment options, like cervical traction or steroid injections, may be considered if surgery is not an option.
The overall goal is to relieve pain, improve quality of life, and prevent further spinal cord or nerve root damage.
Posterior Cervical Fusion
Have you ever wondered about another common procedure for addressing neck issues, known as Posterior Cervical Fusion? This surgical method focuses on the back (posterior) part of the neck. It involves the fusion of two or more cervical vertebrae to stabilize the neck and alleviate pain. Fusion longevity, a critical factor, is determined by numerous variables including patient health, surgical technique, and implant materials used. The primary goal is to achieve solid fusion that lasts a lifetime, minimizing the risk of additional surgery. However, one potential complication is Adjacent Segment Disease (ASD). This condition involves the degeneration of vertebrae next to the fused section, which can cause new symptoms post-surgery and may require further intervention.
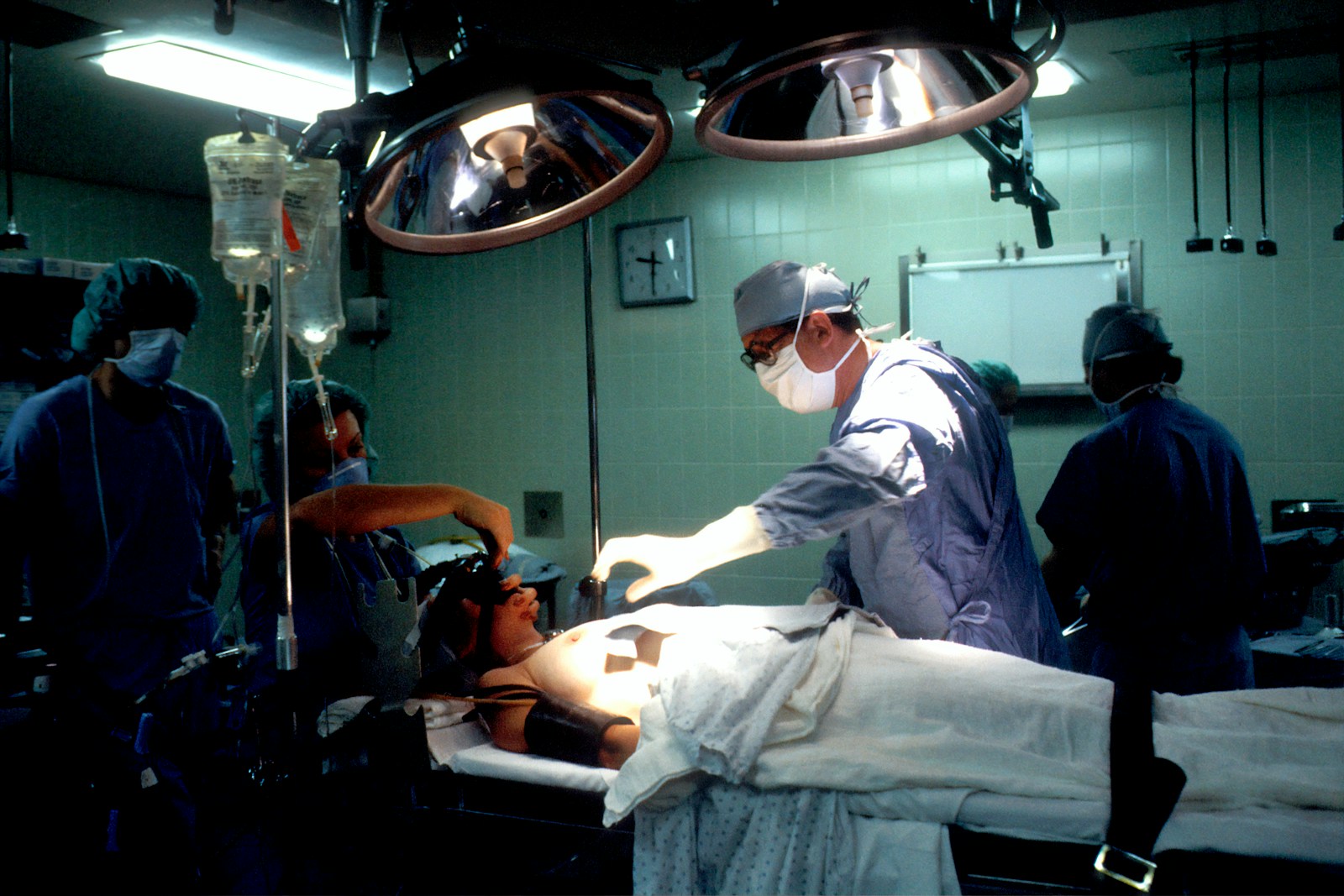
Anesthesia and Patient Positioning
In the intricate process of neck surgery, the initial step is the administration of anesthesia, followed by meticulous patient positioning to guarantee ideal surgical access and patient safety. Anesthesia types vary depending on the surgery type and patient’s health status. The most common types used are general anesthesia and regional anesthesia. General anesthesia renders the patient unconscious, while regional anesthesia numbs a large area of the body.
Patient positioning can pose several challenges. It is important to prevent pressure sores, nerve injuries, and maintain an open airway. Hence, surgeons often use specific positioning devices for optimum neck exposure while ensuring patient safety. The choice of patient position mainly depends on the surgical approach, the patient’s physical condition, and the nature of the pathology.
To summarize, the following points are significant:
- Choice of anesthesia type based on surgery type and patient’s health status
- Prevention of positioning challenges such as pressure sores and nerve injuries
- Use of specific positioning devices for optimum surgical exposure
- Patient position determined by surgical approach, patient’s physical condition, and nature of pathology.
This careful preparation sets the stage for successful neck surgery.
Types of Neck Retractors
Once the patient is correctly positioned and stable, the surgical team turns its attention to the use of neck retractors, an essential tool that aids in the visibility and accessibility of the surgical area. Retractor advancements have led to a variety of types available, each designed for specific surgeries and patient anatomies.
The most common types include the self-retaining retractors, which hold the tissues apart without the need for manual handling. This type provides a clear, unobstructed view of the surgical field, making it a versatile tool in many neck surgeries. There are also handheld retractors, typically used in more delicate or complex surgeries.
The retractor materials must be carefully considered as well. Most retractors are made of stainless steel due to its durability, corrosion resistance, and ability to be sterilized. However, advancements have led to the introduction of silicone and plastic retractors, which are lighter and cause less tissue trauma.
Choosing the right retractor involves understanding the surgical procedure, patient anatomy, and the properties of the retractor materials. This guarantees optimal visibility, improved surgical outcomes, and patient safety. The ultimate goal is to perform the procedure efficiently without compromising the integrity of the surrounding tissues.
Use of Intraoperative Neurophysiological Monitoring
Intraoperative Neurophysiological Monitoring (IONM) is a significant advancement in the field of neck surgery. It serves as a real-time alert system, detecting potential neurological complications during surgical procedures. The subsequent discussion will focus on understanding this technology, its benefits during surgery, as well as associated risks and precautions.
Understanding Neurophysiological Monitoring
During the intricate process of neck surgery, the use of Neurophysiological Monitoring, specifically Intraoperative Neurophysiological Monitoring, plays a pivotal role in ensuring the patient’s neurological integrity. This method encompasses the application of various neurophysiological tools to measure the functional integrity of certain neural structures (nerves, spinal cord and parts of the brain) during surgery.
This encompassing technique involves:
- Applying sensors and electrodes to the patient
- Real-time monitoring of neurophysiological data
- Identification of changes in neural pathways
- Immediate communication to the surgical team about neural integrity
Understanding the monitoring effectiveness of these tools is essential. They not only guide the surgeon during the procedure but also provide an early warning system for potential neurological damage, thereby ensuring the patient’s safety and improving surgical outcomes.
Benefits of Intraoperative Monitoring
The utilization of Intraoperative Neurophysiological Monitoring (IONM) yields substantial benefits in the field of neck surgery, most notably by enhancing patient safety and improving surgical outcomes. Real-time data provided by IONM allows surgeons to make informed decisions during complex procedures, minimizing the risk of neurological damage. Consequently, this provides neurological protection, raising the standard of patient care.
Furthermore, monitoring advancements have made IONM more precise and efficient. The advent of high-resolution neuroimaging, combined with advanced algorithms, has improved the accuracy of neural pathway mapping. This capability not only guides surgeons but also helps to predict possible complications, leading to safer surgery. Ultimately, the use of IONM contributes to better surgical outcomes by reducing postoperative neurological deficits and facilitating faster patient recovery.
Risks and Precautions
Despite the numerous advantages of using Intraoperative Neurophysiological Monitoring (IONM) in neck surgery, it’s critical to acknowledge the inherent risks and essential precautions associated with its use.
- Anesthesia complications: IONM requires a specialized anesthesia protocol to maintain a stable and responsive neurophysiological environment. Any deviation can lead to false positives or negatives, affecting the accuracy of IONM.
- False negatives: Despite precautions, there’s a chance that IONM might not detect all neural damage.
- Technical errors: This includes poor electrode placement, equipment malfunction, or interpretation errors.
- Rehabilitation methods: Post-surgery, patients may require intensive rehabilitation. While IONM can reduce the risk of neural injury, it doesn’t eliminate the need for post-operative care.
Thus, while IONM is a potent tool, understanding its limitations and potential risks is important for excellent surgical outcomes.
Surgical Frames and Neck Support
In the domain of neck surgery, the use of surgical frames and neck supports plays a crucial role in maintaining the stability and safety of the patient’s cervical spine. Recent innovations in supporting devices have focused on improving the biomechanical considerations involved in neck stabilization during surgery.
Such devices are designed to provide excellent exposure of the surgical field while preserving the anatomical integrity of the neck. The biomechanical considerations involve evaluating the patient’s neck biomechanics, the surgical procedure requirements, and the device’s mechanical properties. The aim is to minimize surgical risk while ensuring comfort and stability throughout the procedure.
Surgical frames, for instance, often incorporate head and neck supports with adjustable positioning and secure locking mechanisms for enhanced stability. They accommodate the patients’ individual anatomical variations and the specific demands of the surgery.
Likewise, neck supports are designed to distribute pressure evenly across the neck’s surface, reducing the risk of pressure ulcers and nerve damage. High-density foam and gel materials are commonly used due to their pressure-distributing properties and resilience.

Special Considerations in Neck Surgery
Special considerations in neck surgery encompass a myriad of factors, ranging from the patient’s overall health status to the specific anatomical and physiological characteristics of the cervical spine. The increasing complexity of these operations often demands enhanced surgical tools innovation and improved patient communication methods.
- Surgical tools innovation: Advances in surgical technology have contributed to the increased precision and safety of neck surgeries. Innovations include minimally invasive instruments, computer-assisted navigation systems, and state-of-the-art imaging devices.
- Patient communication methods: Effective communication with the patient before, during, and after the surgery is crucial. This may involve educating the patient about the procedure, addressing concerns, and providing postoperative instructions.
- Patient’s overall health status: The patient’s general health, including any underlying medical conditions, can have a significant impact on the surgery’s outcome. A thorough preoperative assessment is therefore essential.
- Anatomical and physiological characteristics: The unique structure and function of the cervical spine require careful consideration. The surgeon needs to account for the proximity of important structures like the spinal cord and vertebrae, which can influence the surgical approach.
These special considerations ensure the surgery is appropriately tailored to the patient’s needs, paving the way for a successful surgical outcome.
Postoperative Neck Care
After the implementation of the bespoke surgical plan, adept postoperative neck care becomes an essential component of the patient’s recovery process. This involves a structured approach, incorporating pain management and scar healing, to facilitate best possible recovery.
Pain management is the cornerstone of postoperative care. This involves the administration of analgesics and non-steroidal anti-inflammatory drugs (NSAIDs) as per the patient’s condition and tolerance. The focus is on controlling the pain without causing undue side effects, such as nausea or excessive sedation. Regular assessment of pain levels using validated scales assists in delivering personalized pain management strategies.
Scar healing is another critical aspect of postoperative neck care. The application of topical agents and regular cleaning of the surgical site prevents infection and promotes healing. In some cases, silicone-based products may be used to reduce scar visibility. Gentle massage around the scar can also support the healing process by stimulating blood flow.
Moreover, a balance of rest and physical therapy exercises is essential. While rest aids in healing, prescribed exercises maintain neck mobility and prevent stiffness. Regular follow-ups with the surgical team ensure timely identification and management of any postoperative issues, thereby promoting smooth recovery.
Potential Risks and Complications
Despite meticulous planning and execution, neck surgery carries an inherent risk of certain complications, each with its own set of potential implications on the patient’s recovery. Infection control is a critical aspect, as postoperative infections can greatly interfere with the recovery timeline, leading to a longer hospital stay and possible readmission for additional treatment.
The potential risks and complications can include:
- Infection: Despite rigorous infection control measures, patients may still develop infections after surgery. These can be localized to the surgical site or systemic, affecting the entire body.
- Nerve Damage: The neck houses numerous nerves. Accidental injury to these nerves during surgery can lead to temporary or permanent complications such as numbness, pain, or even paralysis.
- Bleeding and Hematoma Formation: Any surgery carries the risk of excessive bleeding or hematoma formation, which can exert pressure on the surrounding structures, causing pain and necessitating further intervention.
- Delayed or Impaired Healing: Certain factors such as age, nutrition, comorbidities, and adherence to postoperative care instructions can impact the recovery timeline, potentially delaying or impairing healing.
Understanding these risks allows for better preparation and management, thereby ensuring favorable patient outcomes.
The Evolution of Neck Surgery Techniques
The trajectory of neck surgery has seen notable advancements over the years, with techniques evolving from rudimentary procedures to sophisticated operations, markedly improving the precision, safety, and efficacy of these surgical interventions. Surgical innovations have been instrumental in this evolution, introducing minimally invasive procedures that reduce trauma to the surrounding tissues, thereby enhancing patient recovery.
These state-of-the-art techniques, such as endoscopic and robotic-assisted surgeries, employ advanced imaging and navigation systems to increase surgical accuracy. The adoption of intraoperative neurophysiological monitoring has further bolstered this precision, mitigating the risk of nerve damage. Additionally, the use of biocompatible materials for implants and grafts has significantly reduced postoperative complications and improved patient outcomes.
Furthermore, the implementation of evidence-based perioperative care protocols, often termed as Enhanced Recovery After Surgery (ERAS) protocols, has revolutionized postoperative care. These involve multimodal analgesia, early mobilization, and optimized nutrition, all of which expedite recovery and shorten hospital stays.
Frequently Asked Questions
What Is the Average Recovery Time After Neck Surgery?
The average recovery time after neck surgery varies, typically ranging from a few weeks to several months. This duration depends on postoperative mobility levels and potential surgical complications, such as infection or nerve damage.
Can Neck Surgery Affect My Ability to Swallow or Speak?
Neck surgery can potentially affect your ability to swallow or speak, causing voice changes and swallowing difficulties. This typically results from nerve damage during the procedure, but it’s usually temporary and improves with rehabilitation.
Are There Any Non-Surgical Alternatives to Neck Surgery?
Yes, non-surgical alternatives to neck surgery include chiropractic treatments and acupuncture. Chiropractic benefits include pain relief and improved mobility, while the effectiveness of acupuncture is notable for reducing chronic neck discomfort and enhancing relaxation.
How Can I Manage Pain After Neck Surgery?
Post-surgery pain can be managed through a combination of pain medication options and physical therapy. Medications may include analgesics or anti-inflammatories, while physical therapy can enhance mobility and strengthen neck muscles, reducing discomfort.
Will My Insurance Cover the Cost of My Neck Surgery?
Insurance coverage for neck surgery depends on individual policy terms. Factors like insurance eligibility and potential out-of-pocket expenses should be carefully reviewed. It’s advised to directly consult with your insurance provider for precise information.