The progression of surgical interventions for neck pain has witnessed a significant transformation with the introduction of artificial disk replacement. As a state-of-the-art procedure aimed at substituting a damaged disk with a synthetic one, it brings forth intriguing possibilities regarding pain reduction and recovery of function. With careful candidate selection, meticulous execution, and a well-structured postoperative plan, the procedure promises a potential revolution in neck pain treatment. However, as we delve into a deeper understanding of this complex procedure, we must consider its potential risks, benefits, and long-term implications.
Understanding Artificial Disk Replacement
To grasp the concept of artificial disk replacement, it is important to first understand that it is a type of spine surgery that involves replacing a painful disk in the neck with an artificial one. This procedure aims to maintain or restore the normal movement and alignment of the spine.
One of the key aspects of artificial disk replacement is the Disk Material Composition. The artificial disk, often made of metal or plastic-like (biopolymer) materials, is designed to mimic the size and function of a natural disk. These materials are biocompatible, implying that they will not cause a negative reaction once implanted into the body.
The Insurance Coverage Implications of this procedure largely depend on the individual’s insurance policy. While some insurers categorize this procedure as experimental, others recognize its efficacy and cover its cost. However, it is always recommended to discuss this with your insurance provider prior to undergoing surgery, as out-of-pocket costs can be substantial.
The Anatomy of the Neck
When exploring the anatomy of the neck, it is crucial to recognize that this intricate structure houses essential components such as the cervical spine, muscles, arteries, veins, glands, and the trachea, all of which work in harmony to facilitate critical bodily functions. The cervical vertebrae, for example, are a chain of seven bones, named C1 through C7, that provide structural support and flexibility to the neck. These vertebrae encase and protect the spinal cord, a delicate structure transmitting neural messages from the brain to the rest of the body.
Furthermore, the neck musculature, including the sternocleidomastoid and trapezius muscles, enable neck movements and stabilize the head. They also contribute to other functions, such as swallowing and speaking. The carotid arteries and jugular veins in the neck are responsible for the transport of oxygen-rich blood to the brain and the return of deoxygenated blood to the heart.
The neck also houses glands, including the thyroid and parathyroid, that play a pivotal role in metabolic regulation. The trachea, situated in the neck, serves as an essential conduit for air passage to the lungs. Understanding these structures’ interconnected roles is fundamental to appreciating the complex nature of the neck’s anatomy.
Causes of Chronic Neck Pain
Chronic neck pain, a pervasive issue with significant impact on quality of life, can stem from a multitude of causes. To fully understand this condition, it is essential to recognize the complex interplay of anatomical, physiological, and pathological factors that may contribute to persistent discomfort. These encompass a broad spectrum, from degenerative diseases like osteoarthritis to traumatic injuries, and from repetitive strain to certain systemic diseases.
Identifying Chronic Neck Pain
In the domain of persistent discomfort, chronic neck pain serves as a prevalent issue, often stemming from a variety of causes such as degenerative disc disease, neck strain, and nerve compression. The process of Neck Pain Diagnosis involves a thorough evaluation of the patient’s medical history, physical examination, and often, imaging studies. These diagnostic tools help in identifying the root causes of the pain, enabling appropriate treatment planning.
While conventional pain relief treatments are commonly utilized, the exploration of Alternative Therapies has also gained momentum in recent years. Techniques such as acupuncture, chiropractic manipulation, and yoga have shown promise in alleviating chronic neck pain. However, it is crucial to consult a healthcare professional prior to initiating such therapies to guarantee safety and effectiveness.
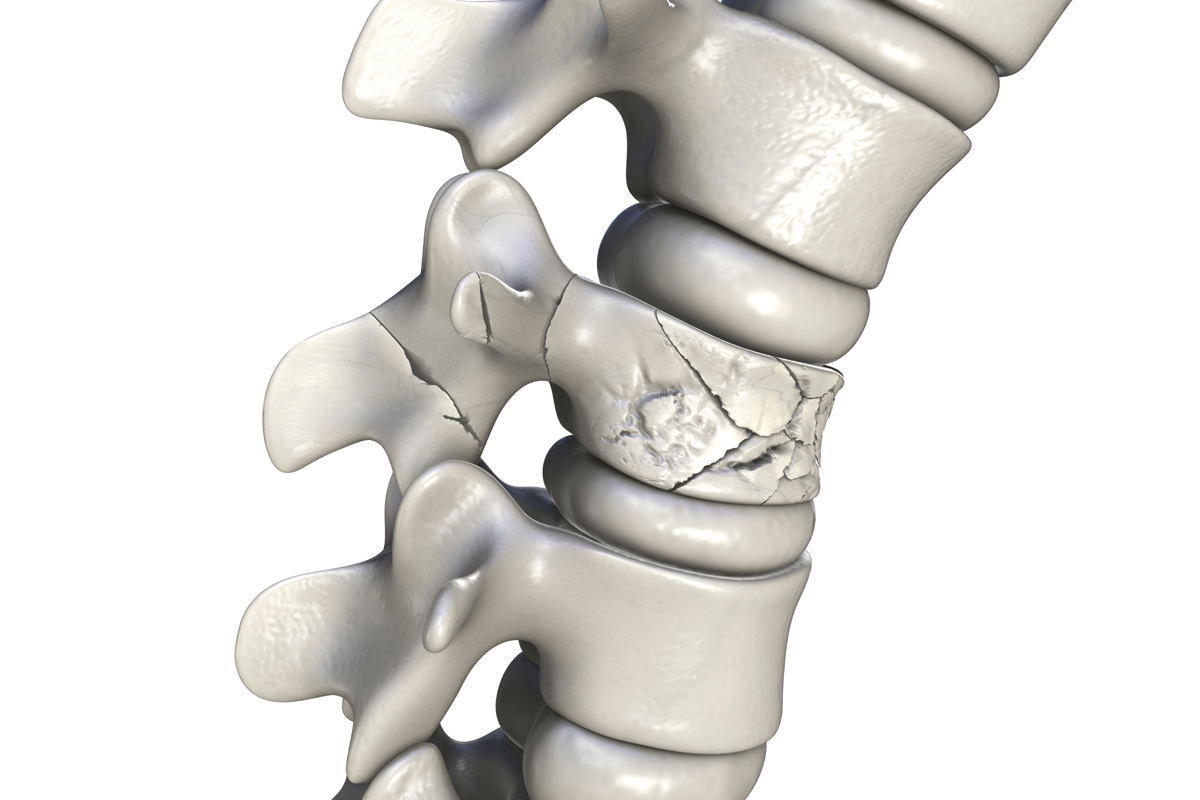
Potential Pain Inducers
Delving into the root causes of persistent cervical discomfort, it is essential to shed light on the potential pain inducers that contribute to chronic neck pain. These inducers often include degenerative disc disease, cervical osteoarthritis, and cervical spinal stenosis. The onset of such conditions can be exacerbated by factors like poor posture, prolonged periods of inactivity, and inadequate ergonomics, all of which compound the need for effective pain management strategies. Lifestyle modifications impact the management of these conditions greatly. Regular exercise, maintaining a healthy weight, and adopting proper ergonomic practices can help alleviate the severity of symptoms. Additionally, medical interventions such as artificial disk replacement have shown promise in providing long-term relief, forming an integral part of thorough pain management strategies.
Traditional Neck Pain Treatments
Over the years, several traditional treatments have been utilized to alleviate neck pain, each with varying degrees of effectiveness and respective drawbacks. These treatments generally fall into four categories:
- Medications: Commonly used drugs include over-the-counter pain relievers, narcotics, muscle relaxants, and even some types of antidepressants. While effective, these can have side effects and the potential for addiction.
- Physical Therapy: This involves stretches and exercises to improve strength and flexibility in the neck. It requires a commitment to a regular routine and may not provide immediate relief.
- Alternative Therapies: Treatments like acupuncture, chiropractic adjustments, and massage therapy can help some individuals. The effectiveness of these methods varies greatly between individuals and is not universally accepted.
- Pain Management Techniques: These can include practices like cognitive behavioral therapy, meditation, or biofeedback, which focus on changing the perception and impact of pain, rather than the physical cause.
Each treatment has its pros and cons, and what works best will depend on the individual patient’s condition and preferences. It’s important for health professionals to explore all options and customize treatments to the individual’s needs and circumstances.

Artificial Disk Replacement: A New Solution
Artificial disk replacement emerges as a pioneering solution in the field of neck pain management, heralding significant advancement in neck surgery. This innovative procedure involves the substitution of a damaged or degenerated cervical disk with an artificial one, designed to maintain or restore spinal motion. Our discussion will elucidate the intricacies of this procedure and the technological advancements that have made it a viable alternative to traditional neck pain treatments.
Understanding Disk Replacement
In order to comprehend the concept of artificial disk replacement, it is imperative to first understand that this innovative surgical procedure serves as a promising solution to chronic neck pain by replacing damaged or degenerated disks with an artificial one. The procedure is a cornerstone in the field of Disk Degeneration Prevention and Spinal Health Maintenance.
- Artificial disks are a biomechanically engineered device designed to mimic the form and function of a natural spinal disk.
- It provides an alternative to spinal fusion surgery, maintaining spinal mobility and potentially halting degenerative changes.
- The artificial disk is inserted between the vertebrae, replacing the damaged disk and providing immediate pain relief.
- Long term outcomes of the procedure may lead to improved quality of life for patients, reduced need for additional surgeries, and a swift return to daily activities.
Neck Surgery Advancements
Pioneering the future of neck surgeries, artificial disk replacement emerges as a revolutionary advancement, offering a novel solution to chronic neck pain and degenerative disk disorders. This procedure is a remarkable surgical innovation that has transformed the landscape of orthopedic surgery. The introduction of this technique has allowed surgeons to maintain the neck’s biomechanics while providing relief and improved mobility.
The artificial disks, made from medical-grade plastic and metal, mimic the natural disk’s function, preserving the neck’s biomechanics and allowing normal neck movement post-surgery. These advancements minimize the risks associated with traditional fusion surgeries, like adjacent segment disease. Considering the rapid pace of surgical innovations, the advent of artificial disk replacement signifies a substantial leap forward, paving the way for future developments in neck surgery.
Selecting the Right Candidates
Patient selection plays a critical role in the success of artificial disk replacement for the neck, with ideal candidates typically presenting with single-level cervical degenerative disk disease refractory to conservative treatment. Patient eligibility and surgery financing are key considerations in this selection process, which must be managed with a high degree of precision and a thorough understanding of the patient’s medical history.
To guarantee successful outcomes, four primary criteria must be considered:
- Clinical Presentation: The patient must exhibit symptoms associated with cervical degenerative disk disease, such as neck pain, radiculopathy, or myelopathy, which are not responsive to non-operative interventions.
- Radiographic Confirmation: Diagnostic imaging should confirm the presence of a degenerative disk that corresponds to the patient’s clinical symptoms.
- Patient Health Status: The patient must be in good overall health, with no contraindications to surgery.
- Financial Readiness: The patient should have access to appropriate surgery financing options, as artificial disk replacement can be a costly procedure.
Preparing for Artificial Disk Surgery
To guarantee a successful outcome of an artificial disk replacement surgery, meticulous preparation is necessary. This involves understanding the surgical procedure and adhering to pre-surgery care measures. Detailed knowledge of the operation and adherence to prescribed pre-operative practices can greatly reduce potential complications and promote expeditious recovery.
Pre-Surgery Care Measures
Before undergoing artificial disk surgery, it is essential to meticulously follow a set of pre-operative care measures to guarantee excellent surgical outcomes. These measures range from pre-surgery nutrition to emotional preparation.
- Pre-Surgery Nutrition: Proper nutrition is crucial to aid in recovery. A balanced diet rich in protein, vitamins, and minerals is recommended. Avoid consuming alcohol or smoking.
- Emotional Preparation: Counseling sessions might be beneficial to mentally prepare for the surgery. Understanding the procedure can alleviate anxiety.
- Physical Preparation: Regular exercise as directed by your surgeon can improve your physical strength and enhance recovery post-surgery.
- Medical Review: Ensure all your medical history, allergies, and current medications are updated and reviewed by the surgical team. This guarantees a personalized approach to your surgery and post-operative care.
Understanding the Procedure
Acquiring a thorough understanding of the artificial disk replacement procedure, from the surgical approach to post-operative care, is vital for ideal preparation and recovery. This surgical process involves removing the damaged disk and replacing it with an artificial one, typically made from medical-grade plastic or metal. The goal is to restore normal neck function and alleviate pain. Concerning Disk Replacement Cost, the price can vary greatly depending on the complexity of the procedure, the material used for the artificial disk, and the patient’s overall health status. Insurance Coverage can help offset these costs, but it’s important to confirm with your provider as not all policies cover this type of surgery. Understanding these factors will assist in better preparation for the procedure.
The Surgical Procedure Explained
Undergoing artificial disk replacement for the neck involves a complex surgical procedure that requires a thorough understanding of the human anatomy, particularly the cervical spine section. Surgical innovations have made this procedure more efficient and less invasive than in the past, but it is still a significant operation.
The procedure generally follows these steps:
- Anesthesia: The patient is first put under general anesthesia to make sure they feel no pain during the procedure.
- Incision: A small incision is made in the front of the neck to access the cervical spine.
- Disk Removal: The damaged disk is carefully removed, taking care not to harm the nearby nerves or spinal cord.
- Artificial Disk Insertion: An artificial disk is then inserted into the empty disk space to replace the removed disk.
Each step is conducted with meticulous care and precision to guarantee excellent results and minimal complications.
Recovery timelines can vary greatly depending on the patient’s overall health and the specifics of their procedure. Patients are typically monitored closely in the immediate postoperative period and given specific instructions for their recovery at home. This procedure represents an important step towards improving the quality of life for patients with chronic neck pain.

Post-Surgery: The Recovery Process
Typically, the recovery process following an artificial disk replacement for the neck involves a carefully structured regimen designed to promote healing, manage pain, and gradually restore mobility. Pain management is typically achieved through a combination of prescription medications and physical therapy.
The importance of physical therapy cannot be overstated. This essential part of the recovery process aids in strengthening the muscles in the neck and improving range of motion, thereby reducing the risk of further injury. Physical therapy is usually initiated a few weeks post-surgery, after the incision has healed, and it is customized to meet the patient’s individual needs.
The question of returning to work is largely dependent on the nature of one’s job. For jobs involving minimal physical exertion, patients may be able to return within a few weeks following surgery. However, for occupations involving heavy lifting or strenuous physical activity, a longer recovery period may be necessary.
It is vital for patients to follow their surgeon’s instructions and adhere to the recommended recovery plan. This will optimize the healing process, ensure the success of the procedure, and expedite the return to normal activities.
Benefits of Artificial Disk Replacement
The implementation of artificial disk replacement offers several significant benefits including improved mobility, reduction in pain, and a quicker return to daily activities. This innovative procedure helps to restore the natural function of the neck, making it a viable option for individuals suffering from chronic neck pain due to degenerative disk disease or other related conditions.
- Disk Durability: Artificial disks are composed of biocompatible materials designed to withstand the rigors of daily activity. They emulate the mechanical properties of natural disks, providing superior durability and longevity.
- Replacement Cost: Despite the initial investment, the cost of artificial disk replacement can be offset by the potential reduction in future medical bills. The elimination of chronic pain and the improvement in quality of life often overshadow the initial expenditure.
- Improved Mobility: The artificial disk allows for natural movement of the neck, providing patients with enhanced flexibility and range of motion.
- Speedy Recovery: Generally, patients experience a faster recovery period compared to traditional spinal fusion surgery. This means returning to work and daily activities in a shorter span of time.
Potential Risks and Complications
Despite the numerous benefits associated with artificial disk replacement, it is essential to take into account potential risks and complications that may arise post-surgery.
Disk Replacement Complications can be broadly classified into immediate and delayed complications. Immediate complications include allergic reactions, hemorrhage, infection, nerve damage, or problems related to anesthesia. Delayed complications may involve device failure, persistent neck pain, or adjacent segment disease, where the segments above or below the replaced disk degenerate.
Risk Management Strategies should be employed to mitigate these complications. Prior to surgery, patients should undergo rigorous health evaluations to assess their fitness for the procedure. Allergies, medical history, and current medication usage should be thoroughly reviewed. During surgery, meticulous surgical technique and careful handling of tissues are essential to minimize nerve damage and blood loss. Postoperatively, surveillance using imaging techniques can help detect early signs of device failure or adjacent segment disease.
Frequently Asked Questions
How Does Artificial Disk Replacement Affect an Individuals Mobility in the Long Term?
Long-term mobility post-procedure largely depends on the individual’s recovery timeline and necessitated lifestyle changes. Successful procedures often enhance mobility and reduce pain, though some individuals may experience varying degrees of lingering stiffness or discomfort.
Are There Any Alternatives to Artificial Disk Replacement for Chronic Neck Pain?
Yes, alternatives exist for chronic neck pain management. These include physical therapy, medication, acupuncture, and disk material innovation procedures. Each offers varying recovery timeframes and effectiveness, and are best considered in consultation with a healthcare professional.
Is There a Specific Age Range That Benefits Most From Artificial Disk Replacement?
There’s no specific age range that benefits most from disk replacement. However, disk replacement risks and recovery timeline may vary, with younger patients generally experiencing quicker recovery and fewer complications post-surgery. Consultation with a specialist is advised.
How Does the Cost of Artificial Disk Replacement Compare to Traditional Neck Pain Treatments?
The cost comparison between artificial disk replacement and traditional pain treatments varies, influenced by factors like insurance coverage and post surgery rehabilitation. Individual case analysis is essential for precise financial implications.
Can Artificial Disk Replacement in the Neck Impact Other Regions of the Spine?
Yes, artificial disk replacement can potentially impact other regions of the spine. Factors such as disk durability and post-surgery recovery play key roles in determining the extent of this impact. Further studies are needed for confirmation.