The intricacies of the cervical facet and its pivotal role in supporting our neck movements remain a compelling topic of discussion. As these joints bear the brunt of daily wear and tear, the potential for degeneration and inflammation increases, leading to a spectrum of cervical facet disorders. By exploring the complexities of this condition, we can better understand its diagnostic procedures, treatment options, and preventative measures, thereby improving the quality of life for those affected. The question then becomes, how do we optimize the health of our cervical facet joints amidst our dynamic and demanding lifestyles?
Understanding the Cervical Facet
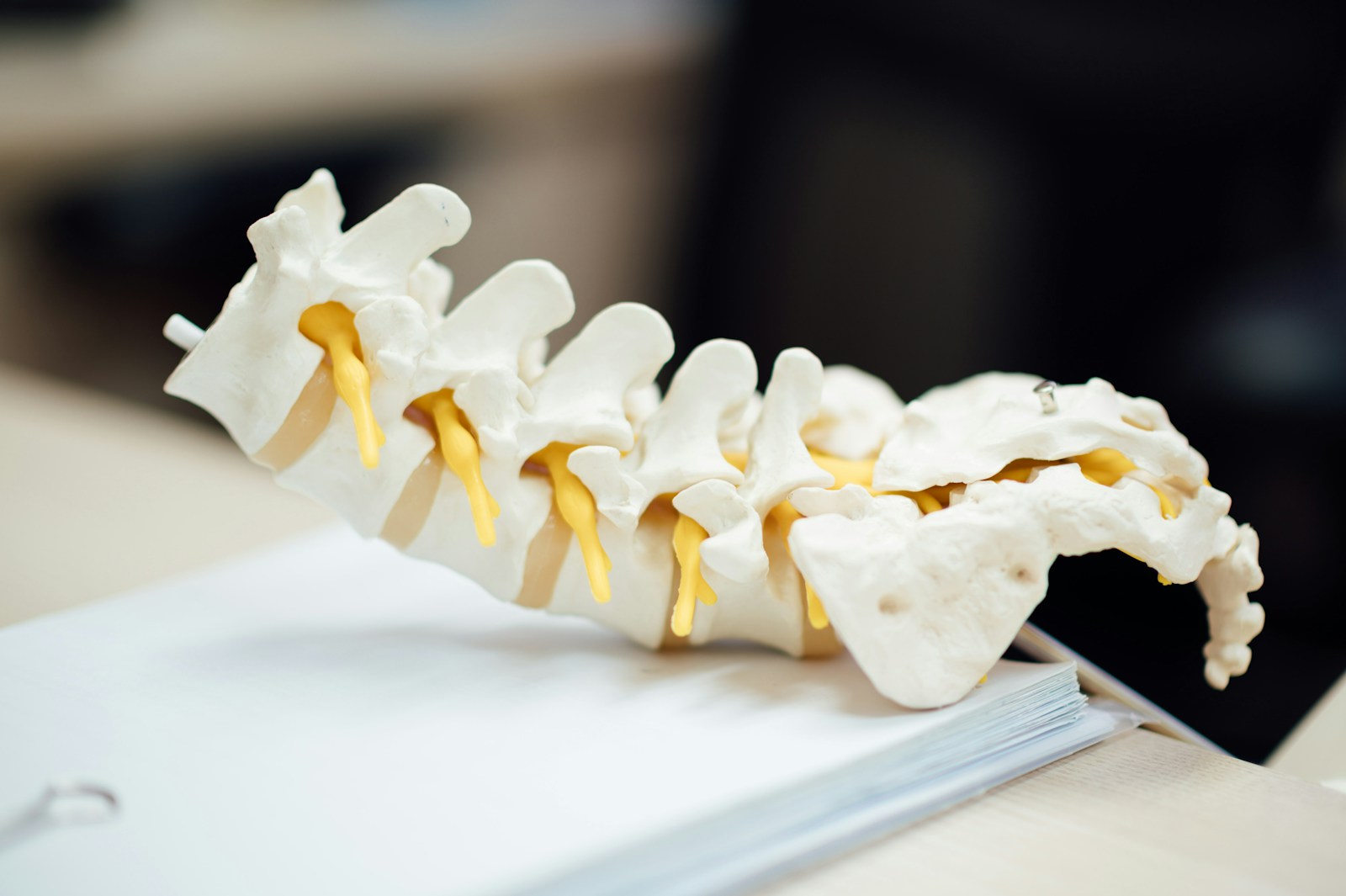
The cervical facet, an integral component of the spinal structure, plays a crucial role in providing stability and facilitating a range of motions in the neck region. Despite its importance, the cervical facet is susceptible to various pathological conditions, especially facet inflammation and facet degeneration, both of which can greatly impact its function and lead to debilitating pain or discomfort.
Facet inflammation causes are multifactorial, typically originating from mechanical stress, injury, or aging. These triggers can incite an inflammatory response within the facet joints, resulting in swelling and pain. Over time, persistent inflammation can cause the facet joints to become hypertrophic, leading to further discomfort and limited mobility.
Facet degeneration, on the other hand, is primarily a consequence of the aging process, although it can be exacerbated by factors such as obesity, poor posture, and genetic predisposition. The degeneration impact is characterized by the breakdown of the cartilage within the facet joints, leading to bone-on-bone contact and resulting in chronic pain, stiffness, and decreased range of motion. Understanding these causes and impacts can aid in the development of effective treatment strategies for cervical facet-related disorders.
Anatomy of Cervical Facet Joints
To fully comprehend the pathology and associated discomfort of cervical facet-related conditions, a detailed understanding of the anatomical structure of the cervical facet joints proves indispensable. The cervical facet joints, also known as zygapophysial joints, are synovial joints located bilaterally on the posterior aspect of the vertebral column. Each facet joint is comprised of two articulating surfaces: the superior articular process of the vertebra below and the inferior articular process of the vertebra above.
These joints are covered by hyaline cartilage which facilitates smooth movement and helps to absorb shock. The joint capsule, a fibrous tissue enclosing the joint, contains synovial fluid that reduces friction during motion. Facet joint degeneration, a common cause of neck pain, is a condition where the cartilage of these joints wears down over time, leading to bone-on-bone contact.
Cervical facet arthritis, another degenerative condition, involves inflammation of the facet joints in the neck. This can lead to stiffness, pain and potentially, a reduction in the range of motion. Understanding the intricate anatomy of cervical facet joints is fundamental in the diagnosis and treatment of these conditions.
Role of Cervical Facets in Movement
Integral to the mobility and flexibility of the neck, cervical facet joints permit a variety of movements including rotation, flexion, and extension, while simultaneously providing significant stability to the spinal column. The intricate articulation of these joints facilitates a complex range of motion, allowing for the transmission of forces and movements in multiple planes.
The importance of these joints is paramount to their function. Facet inflammation causes such as osteoarthritis or trauma can lead to swelling, pain, and a reduction in mobility. This inflammation is often a result of the wear and tear of the articular cartilage, which exacerbates friction between the joint surfaces and may lead to facet joint degeneration.
Degenerative changes in the facet joints can severely limit neck mobility. As the articular cartilage thins and the joint space narrows, the range of motion decreases and the joints lose their ability to glide smoothly. Additionally, the body may respond to this degeneration by forming bone spurs, or osteophytes, which further restrict movement and may cause nerve impingement.
Thus, maintaining the health of the cervical facets is essential for ensuring the full range of neck motion and overall spinal stability.
Common Cervical Facet Disorders
Despite the pivotal role of cervical facets in movement and spinal stability, they are susceptible to a number of disorders, such as osteoarthritis, facet joint syndrome, and cervical disc herniation, which greatly impede their function and the overall quality of life.
Facet arthritis, one of the primary disorders, is often spurred by age-related degeneration and chronic wear and tear. The primary cause of facet arthritis is the cartilage break-down within the facet joints, leading to inflammation and pain. Another common disorder is facet joint syndrome, often resulting from stress and strain on the cervical facets, leading to joint degeneration. Degenerative changes can cause the joint’s protective cartilage to erode, causing bone-on-bone contact—a key contributor to persistent pain and limited mobility.
Cervical disc herniation, another prevalent disorder, occurs when the soft central portion of a spinal disc bulges out through a tear in the tougher outer layer. This can place pressure on nearby nerves, leading to pain and potentially serious neurological symptoms. Understanding these disorders is essential for appropriate diagnosis and management of cervical facet-related conditions, ensuring excellent patient outcomes.
Symptoms Indicating Cervical Facet Issues
When cervical facet disorders manifest, they typically present a variety of symptoms that can greatly affect a patient’s daily life, including chronic neck pain, stiffness, headaches, and in severe cases, radiating pain to the shoulders and arms due to nerve compression. This array of symptoms often leads patients to seek medical intervention, which may include facet joint injections as a possible treatment option.
Facet joint injections, a minimally invasive procedure, are often utilized for both diagnostic and therapeutic purposes. They can provide temporary relief from the debilitating symptoms, and if successful, may indicate that the facet joints are the source of discomfort.
Other symptoms may include reduced range of motion, difficulty in maintaining an upright posture, and a significant decrease in the quality of life due to persistent pain. The pain may exacerbate during certain activities like turning the head or bending the neck, further indicating cervical facet issues.
Alternative therapy options are also available for patients who may not respond to traditional treatments or those desiring a non-invasive approach. These may encompass physical therapy, chiropractic adjustments, acupuncture, and lifestyle modifications. Each symptom and its severity play a critical role in determining the most appropriate treatment method, hence, a thorough patient evaluation is paramount.
Diagnosing Cervical Facet Conditions
In the thorough diagnostic process of cervical facet conditions, the initial step involves the recognition of the characteristic symptoms. This is followed by a detailed medical examination, often employing an array of specific procedures to evaluate the severity and exact location of the problem. Advanced imaging techniques, such as MRI or CT scans, are then typically utilized to provide a more detailed view of the cervical spine and further clarify the diagnosis.
Identifying Cervical Facet Symptoms
Unearthing the symptoms of cervical facet conditions requires a meticulous understanding of the anatomy and physiology of the cervical spine, along with a keen attention to the patient’s clinical presentation and history. Facet arthritis progression is often a key indicator, along with other symptoms which can be identified through a holistic pain management approach.
The common symptoms of cervical facet conditions include:
- Persistent neck pain that may radiate to the shoulders or upper back
- Limited range of motion in the neck
- Headaches originating at the base of the skull
- Increased discomfort when leaning or turning the head
- Tenderness over the affected facet joint
Recognizing these symptoms early can lead to more effective treatment strategies, and potentially slow the progression of facet arthritis.
Medical Examination Procedures
To accurately diagnose cervical facet conditions, medical practitioners adopt a thorough approach, utilizing an array of clinical examination procedures, radiographic imaging techniques, and occasionally, diagnostic injections. They employ pain management techniques, ranging from pharmaceutical interventions to alternative therapies, to assess the patient’s response and further refine the diagnosis. A detailed patient history and physical examination, focusing on the cervical spine, are conducted to identify any symptom patterns. Palpation and range of motion tests can also offer insights into the potential involvement of the cervical facet joints. Diagnostic injections, although invasive, are sometimes used to confirm the source of pain. Alternative therapies, such as acupuncture or chiropractic manipulations, might also provide valuable diagnostic information, based on the patient’s symptom relief.
Imaging Techniques Used
Peering into the complexities of the cervical facet conditions, radiographic imaging techniques play an indispensable role in providing an in-depth visualization of the cervical spine architecture and its potential anomalies. The radiographic analysis aids in identifying degenerative changes, fractures, and dislocations that commonly manifest in cervical facet syndromes.
The following imaging techniques are frequently utilized:
- X-Ray : This standard radiographic imaging allows visualization of bony structures and alignment.
- CT Scan : Offers detailed images of the cervical vertebrae.
- MRI : Ideal for visualizing soft tissues including the spinal cord and nerve roots.
- Myelography : Involves injection of a contrast medium to enhance the imaging of spinal cord and nerve roots.
- Discography: Contrast enhancement techniques are used to identify painful disc levels.
These tools provide a thorough understanding of the cervical facet conditions.
Non-Surgical Treatment Options
Often, patients diagnosed with cervical facet syndrome can explore various non-surgical treatment options, which may include physiotherapy, medication management, and lifestyle modifications, designed to alleviate symptoms and improve quality of life. Among the wide range of available pain management techniques, physiotherapy remains a frontline non-surgical intervention. It employs strategic exercises to strengthen neck muscles, improve posture, and increase flexibility, thereby reducing pressure on the cervical facet joints.
Medication management is another critical component of non-surgical treatment. It involves the use of non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or corticosteroid injections. These pharmaceutical agents work to reduce inflammation, alleviate pain, and enhance mobility.
Alternative therapy options such as acupuncture, chiropractic adjustments, and massage therapy are also beneficial. These techniques can complement traditional treatments, offering additional relief by targeting specific pain points, improving circulation, and promoting overall wellness.
Lifestyle modifications, such as weight management and cessation of smoking, are also integral to managing cervical facet syndrome. These interventions focus on mitigating external factors that can exacerbate the condition’s symptoms.
Surgical Interventions for Cervical Facet Pain
Exploring the realm of surgical interventions for cervical facet pain, it becomes clear that these procedures, ranging from minimally invasive nerve blocks to more extensive cervical fusion surgeries, offer a significant potential for effective pain management in patients for whom non-surgical treatments have proven insufficient.
There are several key points to keep in mind:
- Minimally invasive nerve blocks: These procedures involve the injection of a local anesthetic to numb the affected nerves, providing immediate relief.
- Radiofrequency ablation: This procedure uses heat generated by radio waves to target and disrupt nerve function, preventing the transmission of pain signals to the brain.
- Cervical facet joint injections: Steroids are administered directly into the facet joint to reduce inflammation and alleviate pain.
- Cervical fusion surgery: In more severe cases, this procedure is used to permanently connect two or more bones in the spine, providing long-term stability and pain relief.
- Postoperative complications: Like any surgical intervention, these procedures carry potential risks, including infection, bleeding, and adverse reactions to anesthesia.
Patient recovery varies depending on the surgical option employed, the individual’s overall health, and the effectiveness of postoperative care. Each intervention requires a thorough understanding of the cervical spine’s anatomy, surgical techniques, and the potential for complications to ensure favorable outcomes.

Rehabilitation After Cervical Facet Surgery
After the surgical interventions for cervical facet pain, an essential phase is the thorough rehabilitation process, which is meticulously designed to promote healing, restore function, and prevent re-injury. This multidimensional approach encompasses physical therapy, post-operative nutrition, and emotional coping strategies.
Physical therapy focuses on enhancing neck mobility, strengthening muscles, and improving posture. It may involve a combination of exercises, manual therapy, and electrotherapy. The goal is to alleviate pain, restore range of motion, and improve the patient’s ability to perform daily activities.
Post-operative nutrition plays a significant role in the healing process. A balanced diet rich in proteins, vitamins, and minerals aids in tissue repair, decreases inflammation, and boosts the immune system. Adequate hydration is also crucial for optimal recovery.
Emotional coping strategies are integral to rehabilitation. Postoperative patients often experience anxiety, depression, or fear due to pain, functional limitations, or potential complications. Psychological interventions, such as cognitive-behavioral therapy, can help patients manage these emotions, promoting a positive mindset and enhancing overall recovery.
Thus, a thorough rehabilitation plan, addressing both physical and emotional aspects, is pivotal in ensuring successful recovery following cervical facet surgery.
Preventive Measures for Cervical Facet Health
Implementing preventive measures for cervical facet health, such as the incorporation of regular physical activities and the practice of proper posture, are paramount in the maintenance of spinal integrity. Regular physical activities, particularly those that strengthen the neck and upper back muscles, can enhance cervical stability and alleviate undue stress on the facet joints. Similarly, the maintenance of a healthy posture, specifically in activities of daily living and occupational tasks, plays a critical role in mitigating the risk of cervical facet degeneration.
Regular Physical Activities
Engaging in regular physical activities serves as an essential preventive measure to maintain cervical facet health, enhancing flexibility and strength in the neck area, thereby reducing the likelihood of injuries and disorders. The exercise benefits are innumerable, extending beyond mere physical wellness to aspects such as improved mental health, reduced stress, and better sleep patterns. However, it’s important to understand the activity limitations to avoid overexertion, which might lead to unwanted injuries.
- Aerobic activities improve cardiovascular health and increase neck mobility.
- Strength training exercises promote muscle endurance and prevent degradation of cervical facets.
- Balance and flexibility exercises help in maintaining proper alignment and reducing the risk of falls.
- Low impact exercises like swimming and walking can be beneficial for people with existing neck conditions.
- Regular breaks and stretching during long periods of inactivity also contributes significantly to cervical facet health.
Healthy Posture Maintenance
Adopting a healthy posture, particularly while performing daily activities, is an essential preventive measure for preserving cervical facet health, as it reduces undue stress on the neck, promotes proper alignment of the spine, and minimizes the risk of developing neck-related conditions and disorders.
Incorporating posture correction tools such as lumbar rolls and ergonomic chairs can facilitate ideal postural alignment, thereby mitigating the incidence of cervical facet degeneration. Additionally, an ergonomic workspace design that includes adjustable desks and computer screens at eye level can further contribute to maintaining a healthy posture. Regular posture checks, preferably with professional guidance, can also be instrumental in identifying and correcting postural deviations. Cumulatively, these measures can enhance cervical facet health by promoting postural integrity and reducing undue biomechanical loading.
Living With Chronic Cervical Facet Pain
Managing chronic cervical facet pain requires a thorough understanding of the condition, a commitment to lifestyle modifications, and possibly ongoing medical interventions. The application of pain management strategies is essential, and the inclusion of emotional coping techniques can be beneficial for overall wellbeing.
Living with chronic pain derived from cervical facet syndrome demands a multi-pronged approach:
- Education: Understanding the nature of the condition, its causes, and potential triggers can help patients make informed decisions about their lifestyle and treatment options.
- Physical Therapy: Regular, targeted exercises can strengthen neck muscles, improve mobility, and reduce pain.
- Medication: Non-steroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or even corticosteroid injections can be utilized to control pain levels.
- Lifestyle Adjustments: Modifying daily activities to avoid exacerbating the condition. This could mean ergonomic adjustments at work, changing sleeping positions, or avoiding certain physical activities.
- Emotional Support: Chronic pain can strain mental health. Emotional coping techniques such as cognitive-behavioral therapy, mindfulness, or support from loved ones can play an important role in maintaining a positive outlook.
Frequently Asked Questions
What Is the Average Recovery Time After Cervical Facet Surgery?
The recovery period after surgery varies among individuals, typically ranging from weeks to several months. This timeframe can be influenced by factors such as facet injection benefits and potential surgery complications.
How Does Aging Impact the Health of Cervical Facet Joints?
Aging can greatly impact joint health due to dietary influence and genetic factors. With age, cartilage wears down, causing joint stiffness and pain. Additionally, genetic predispositions can exacerbate these degenerative changes, impacting overall joint health.
Are There Any Specific Exercises to Strengthen the Cervical Facets?
Yes, specific exercises can promote Facet Nutrition and mitigate Cervical Facet Stress. These include neck stretches, isometric exercises, and cervical extension activities, all of which strengthen supportive muscles and enhance joint health.
Can Poor Posture Lead to Cervical Facet Disorders?
Yes, poor posture can contribute to the development of facet disorders. Posture correction techniques play a significant role in facet disorders prevention, helping to maintain spine alignment and reduce undue pressure on facet joints.
Are Certain Professions at Higher Risk for Cervical Facet Issues?
Yes, professions involving prolonged static postures, repetitive neck movements, or heavy physical work are at an increased risk. Early diagnosis of facet syndrome and preventive measures are essential in these high-risk occupations.

