The intricacy and potential utility of the medial branch block procedure warrant a thorough discussion. This diagnostic tool, which involves the targeted injection of anesthetic near spinal nerves, has shown promise in the management of chronic back pain. However, as with any medical intervention, it is important to understand its mechanism, benefits, potential risks, and overall success rate. This discussion will provide insights into these aspects, inviting further exploration of this intriguing subject.
Understanding Medial Branch Block
Grasping the concept of Medial Branch Block involves understanding its role as a diagnostic procedure that is used to determine whether a specific set of spinal nerves, often associated with arthritic conditions, is the source of a patient’s back pain. This process is often employed when conventional techniques fail to identify the root cause of discomfort.
The effectiveness of the Medial Branch Block is often determined by the amount of pain relief experienced post-procedure. If the patient’s pain is greatly reduced or eliminated, it indicates that the targeted nerves were indeed the source of pain. However, this process is not infallible and may require multiple attempts to accurately identify the troubled nerves.
Alternative treatments are also available for patients who do not respond positively to the block or for whom the procedure is considered inappropriate. These might include physiotherapy, pain management medication, and in some cases, surgical intervention. However, these alternatives aren’t without their limitations and potential side effects.
The Anatomy Involved
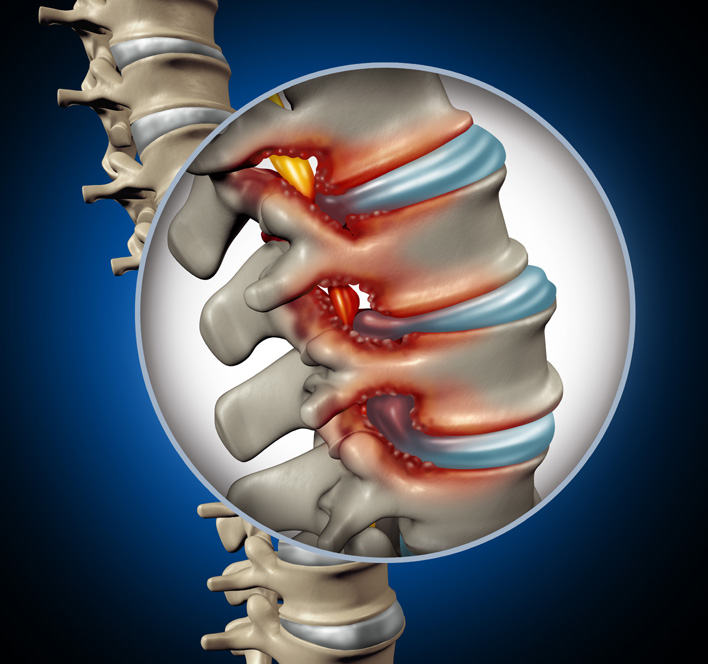
A thorough understanding of the anatomy involved in Medial Branch Block necessitates a detailed examination of the spine, specifically the medial branch nerves. These nerves, originating from the dorsal ramus, innervate the facet joints, multifidus muscles, interspinous ligaments, and the skin overlying the spinal processes.
In the context of nerve pathways exploration, it’s vital to highlight the specific pathway of these nerves. Beginning at the spinal cord, they traverse through the foramina or natural openings in the spine. They then branch out, supplying innervation to the aforementioned structures. Understanding these pathways is essential in order to comprehend the blockage mechanics involved in a Medial Branch Block.
These blocks are performed by injecting an anesthetic around the medial branch nerves to interrupt the pain signal from the facet joints. This necessitates a deep knowledge of the spinal anatomy to ensure precise needle placement. The particularities of the bony structure, the location of the nerves, and the potential for variation among individuals all play a significant role in the execution of this procedure.
The Role of Medial Branch Nerves
The medial branch nerves play an instrumental role in the transmission of sensory information from the facet joints to the brain, thereby contributing greatly to spinal functions. These nerves are part of the complex network of peripheral nerves, which serve as pathways for the conduction of sensory and motor impulses. Their significance becomes even more palpable when discussing spinal pain, a condition often related to the disruption or irritation of these very nerves.
Nerve conduction studies have been instrumental in elucidating the functions of medial branch nerves. They provide insights into the speed and strength of signal transmission, shedding light on the health and integrity of these nerves. Anomalies in conduction properties can indicate potential nerve damage or disease, which may be the cause of certain pain syndromes.
Interventional radiology plays a significant part in the management of conditions associated with medial branch nerves. Techniques such as medial branch block, where a local anesthetic is injected to numb the nerve, are employed to diagnose and treat pain originating from the facet joints. Understanding the role of medial branch nerves is critical in tailoring appropriate interventions and improving patient outcomes.
Identifying Suitable Candidates
Determining the appropriate candidates for a Medial Branch Block involves a rigorous process that includes careful diagnosis criteria, pain history evaluation, and a thorough physical examination. Each of these steps is paramount in accurately identifying patients who will benefit most from this procedure. By focusing on these key areas, healthcare professionals can guarantee the treatment is applied to those with the highest probability of positive outcome.
Diagnosis Criteria
Identification of ideal candidates for medial branch block hinges on specific diagnosis criteria that encompass a range of factors. It is essential to dispel medial branch myths, such as the misconception that all back pain patients are suitable for this procedure. In reality, only a subset with certain conditions, such as facet joint pain, are appropriate candidates. Diagnostic criteria include physical examination findings, pain patterns, and radiological evidence. Treatment alternatives should also be considered. For example, patients with comorbidities or those who do not respond to conservative treatments could be potential candidates. However, the decision should always be based on a thorough, individualized assessment of the patient’s condition, symptoms, and overall health status.
Pain History Evaluation
In evaluating a patient’s suitability for a medial branch block, a thorough review of their pain history plays a crucial role. It’s essential to identify the source of pain accurately. This requires a detailed understanding of the patient’s pain pattern, including the location, severity, duration, and any triggering factors. Chronic pain prevalence also demands consideration, as persistent pain might indicate a more complex condition that may not respond well to a medial branch block.
The exhaustive pain history evaluation helps in narrowing down the possibilities of the pain origin, facilitating a more targeted approach. It also aids in distinguishing patients who would benefit from the medial branch block from those who wouldn’t, thereby ensuring a higher success rate for the procedure.
Physical Examination Importance
Beyond the pain history evaluation, a thorough physical examination serves as an essential tool in identifying patients who are most likely to benefit from a medial branch block. This examination prominently includes evaluating patients’ posture and conducting a meticulous neurological assessment. Examining posture can reveal abnormal spinal alignments that may contribute to pain, indicating a potential benefit from the procedure. Similarly, a detailed neurological evaluation helps to pinpoint any potential nerve involvement, which again, may be effectively treated with a medial branch block. Hence, the significance of a detailed physical examination is paramount. It allows physicians to determine the underlying source of the pain and identify those patients who are suitable candidates for a medial branch block, thereby enhancing the overall success rate of this treatment modality.
The Benefits of Medial Branch Block
The benefits of the Medial Branch Block procedure are manifold and significant, offering both physical and psychological relief. The most immediate and tangible advantage is the alleviation of chronic pain, which directly contributes to improved mobility for the patient. In addition, by reducing chronic pain, this procedure can considerably diminish the psychological stress often associated with long-term discomfort.
Pain Relief Benefits
Among the numerous advantages, the most significant benefit of Medial Branch Block is its compelling capacity for pain relief. This therapeutic procedure offers a substantive alternative to other treatments, often yielding impressive results.
- Insurance Coverage: Most health insurance policies typically cover this procedure, making it accessible for those in need.
- Reduced Dependency on Pain Medication: It lessens reliance on opioid medications, which often have side effects.
- Quick Relief: Patients usually experience immediate pain relief, enhancing their quality of life.
- Diagnostic Value: Besides providing relief, it helps identify the exact source of pain.
Improving Mobility Aspect
An often neglected yet substantial advantage of Medial Branch Block is its potential to greatly improve mobility in patients suffering from chronic pain. This Mobility Enhancement is pivotal in regaining a good quality of life, allowing patients to resume activities they once enjoyed. The precise delivery of medication to the medial branch nerves interrupts pain signals, thereby alleviating discomfort and facilitating movement. This leads to increased flexibility and strength, which in turn promotes Activity Resumption. The process contributes to a virtuous circle of improvement, as increased physical activity can further reduce pain, enhance muscle tone, and improve overall physical health. Medial Branch Block, consequently, not only manages pain but also offers a holistic approach to patient wellness by improving the mobility aspect.
Psychological Impact Reduction
In addition to its physical benefits, Medial Branch Block greatly reduces the psychological impact often associated with chronic pain. This reduction can be attributed to several key factors:
- Pain Relief: The procedure alleviates pain, leading to improved mental well-being and a significant reduction in stress levels.
- Emotional Resilience: With less pain to manage, patients can focus more on building emotional resilience, which is vital in dealing with chronic conditions.
- Improved Sleep: Chronic pain often disrupts sleep patterns. A reduction in pain promotes better sleep, which is essential for mental wellness.
- Increased Activity: With pain no longer a constant barrier, patients can engage more in activities they enjoy, thereby boosting their mood and overall psychological health.
In essence, Medial Branch Block enhances not just physical, but also mental wellness.
The Procedure: Step by Step
To comprehend the process of a medial branch block, it is important to examine each step meticulously. The procedure generally begins with the patient lying face down on a specialized table. The area of the back where the needle will be inserted is cleaned and sterilized. A local anesthetic is then applied to numb the region.
Under the guidance of fluoroscopy, a real-time x-ray, the physician precisely injects the needle near the medial branch nerves. A contrast dye is used to confirm the correct placement. Subsequently, a mixture of anesthetic and steroid is delivered to reduce inflammation and block the nerve signals. The entire procedure takes about 30 minutes, followed by a short recovery period.
The cost of the procedure varies depending on multiple factors such as geographic location, the anesthesiologist’s fees, and facility charges. Generally, the cost ranges from $1,000 to $2,500. Insurance coverage depends on the specific plan and provider, but typically, if the procedure is deemed medically necessary, a significant portion of the cost is covered. It is advisable to discuss this with your insurance provider to understand the exact out-of-pocket expenses.
Potential Risks and Complications
Like any medical procedure, a Medial Branch Block carries certain potential risks that need to be thoroughly understood. It is crucial to not only identify these possible risks but also comprehend the various complication scenarios that could arise. In the following section, we will succinctly analyze these aspects to provide a thorough understanding of the potential risks and complications associated with a Medial Branch Block.
Identifying Possible Risks
While the Medial Branch Block procedure is generally considered crucial, it is not without potential risks and complications that should be thoroughly understood by the patient. Risk mitigation strategies and aftercare are essential in dealing with these risks.
- Infection: As with any invasive procedure, there is a risk of infection. Sterile techniques are used to minimize this risk.
- Bleeding: Although rare, there can be a risk of bleeding. Patients on blood thinners should notify their doctor before the procedure.
- Nerve Damage: There’s a slight chance of nerve damage during needle insertion. Skilled professionals and precise techniques are employed to mitigate this risk.
- Allergic Reactions: Some patients may have allergic reactions to the medications used. Pre-procedure allergy testing can help avoid this.
Understanding Complication Scenarios
Delving deeper into the potential complications of the Medial Branch Block procedure, it becomes critical to comprehend the various scenarios that could arise, further emphasizing the need for thorough patient education and risk mitigation. Complication prevention is an integral part of post procedure care; it primarily includes monitoring for signs of infection, bleeding or nerve damage. Sometimes, patients may experience increased pain, allergic reactions to the medication, or even a temporary increase in nerve pain. In rare cases, complications might escalate to severe issues like paralysis or stroke. However, a well-informed patient, being vigilant about changes in their condition and seeking timely medical help, can greatly reduce these risks. The role of healthcare providers in ensuring effective patient communication and prompt intervention cannot be overstated.
What to Expect After Treatment
After undergoing a medial branch block procedure, patients may experience a range of outcomes, depending largely on their individual circumstances and the specific nature of their condition. The post-treatment lifestyle may vary greatly amongst patients and is deeply influenced by their commitment to following the prescribed rehabilitation strategies.
The following is a numeric list of four general expectations post-treatment:
1. Pain relief: The primary goal of a medial branch block is to provide pain relief. Patients often experience a notable reduction in their discomfort levels, allowing them to resume normal activities.
2. Rehabilitation: Patients should engage in a structured rehabilitation program, which may include physical therapy and exercise, to strengthen the affected area and prevent recurrence of pain.
3. Lifestyle changes: Patients may need to make certain lifestyle modifications, such as maintaining a healthy weight and avoiding activities that exacerbate their condition, to optimize the effectiveness of the treatment.
4. Follow-up appointments: Regular follow-up visits to the doctor are important to monitor progress and adjust treatment plans as necessary.

Success Rate of Medial Branch Block
When evaluating the effectiveness of the medial branch block procedure, it’s important to take into account its success rate. The block efficacy is often tied to the skill and experience of the medical practitioner, as well as the patient’s unique response to treatment.
Research indicates that the success rate of the medial branch block is generally high, with many patients reporting substantial relief from chronic pain and improved quality of life. The exact rate varies across studies, with estimates ranging from 70% to 90%. This wide range is reflective of the complexity of pain management and the individual variability in patients’ responses.
The recovery timeline also plays a pivotal role in gauging the success of the procedure. Most patients experience relief from pain immediately following the procedure, with the effects lasting from a few months up to a year. The duration of relief is dependent on several factors, including the severity and location of pain, and the patient’s overall health.
Importantly, the success rate of the medial branch block should be evaluated alongside other measures of effectiveness, such as patient satisfaction and improvement in functional status. This holistic approach to evaluation can provide a more thorough understanding of the procedure’s impact on patients’ lives.
Comparing Other Pain Management Procedures
In order to fully appreciate the value of the medial branch block, it is essential to contrast it with alternative pain management procedures, weighing the benefits, risks, and efficacy of each approach. The comparative effectiveness of these procedure alternatives provides us with a broader perspective on pain management.
- Steroid Injections: These are often used to reduce inflammation and pain. However, their effectiveness varies and they can have side effects such as infection and increased blood sugar levels.
- Radiofrequency Ablation (RFA): This involves using heat to disrupt nerve function and reduce pain. While it has shown good results, it is a more invasive procedure than the medial branch block.
- Physical Therapy: This non-invasive approach can help improve mobility and relieve pain over time. Its effectiveness is highly dependent on the patient’s commitment and the nature of the underlying issue.
- Surgery: As a last resort, surgery can be considered. This is usually more effective for structural issues but comes with higher risks and longer recovery times.
Personal Stories: Patient Experiences
Drawing from a wealth of personal narratives, it becomes clear that patient experiences with medial branch block vary widely, reflecting the unique complexities of individual pain management journeys. A common thread, however, is the importance of patient support during the procedure and the subsequent recovery period. The impact of a strong support system should not be underestimated, with many patients attesting to its importance in managing the emotional aspects of their medical journey.
Post treatment lifestyle changes also play a critical role in the overall experience and recovery process. Adjustments often involve physical activities, diet, and stress management techniques, all of which contribute to a holistic pain management approach. Some patients report a remarkable improvement in their quality of life, while others might require additional interventions due to persistent pain.
Despite these varying accounts, it remains evident that the medial branch block procedure, coupled with robust patient support and appropriate lifestyle modifications, can greatly enhance pain management avenues. Therefore, it is important to approach each case individually, utilizing patient experiences to inform and optimize treatment strategies.
Frequently Asked Questions
How Much Does a Medial Branch Block Procedure Typically Cost?
The cost of this particular procedure can vary widely depending on factors such as geographical location and insurance coverage. Procedure risks and recovery time are also essential considerations when evaluating the overall expense of the treatment.
Is This Procedure Covered by Health Insurance?
The coverage of any medical procedure by health insurance largely depends on the individual policy. However, with appropriate Insurance Negotiation Tips and understanding of Coverage Exceptions, one can potentially secure coverage for needed treatments.
Are There Any Lifestyle Changes Needed Before Undergoing the Procedure?
Before any procedure, certain lifestyle changes might be necessary for best results. This can include adjustments in nutrition and daily habits. The specifics, however, largely depend on the individual’s health and the specific procedure.
Can Medial Branch Block Be Repeated if the Pain Reoccurs?
Yes, the procedure can be repeated if pain returns. However, the block’s effectiveness may vary with each application. Post-procedure activities should be monitored and adjusted to prevent aggravating the condition and prolong relief duration.
What Are the Alternatives if Medial Branch Block Is Unsuccessful?
If the initial treatment proves unsuccessful, alternative treatments with varying efficacy exist, such as physical therapy, medication management, spinal cord stimulation, or radiofrequency ablation. These non-surgical options can provide significant relief from chronic pain.