The concept of spinal decompression, a non-surgical therapy for chronic back pain, has been gaining attention in medical circles for its potential benefits and cost-effectiveness. This procedure, which involves controlled movements to relieve pressure on spinal discs, may offer a viable alternative to invasive surgeries or long-term medication. However, with this new focus comes a range of questions. What exactly is spinal decompression, how does it work, and what are the potential risks and benefits? These are the critical issues that warrant a deeper exploration.
Understanding Spinal Decompression
Spinal decompression, a non-surgical therapy aimed at relieving back pain and associated conditions, involves a series of precisely controlled movements that relieve pressure on the discs within the spine, thereby promoting ideal healing in a pain-free and non-invasive manner. This therapeutic intervention, primarily employed for treating disc injuries in the neck and lower back, demonstrates considerable efficacy in alleviating pain and improving the quality of life for patients.
Decompression cost analysis reveals that this non-surgical method is relatively less expensive when compared with the cost of surgical interventions. The financial implications of spinal decompression are mainly linked to the duration of the therapy and the severity of the condition. Despite the repetitive nature of the sessions, the overall cost remains significantly lower than that of invasive surgical procedures.
In comparison, decompression versus surgery demonstrates a stark contrast not only in cost but also in recovery time and potential risks. Unlike surgery, spinal decompression does not pose a risk of infection, blood clots, or nerve damage. Additionally, the recovery period is notably reduced, allowing patients to resume their normal activities sooner. Hence, spinal decompression serves as an efficacious, cost-effective, and safer alternative to surgical interventions for disc-related conditions.
The Need for Spinal Decompression
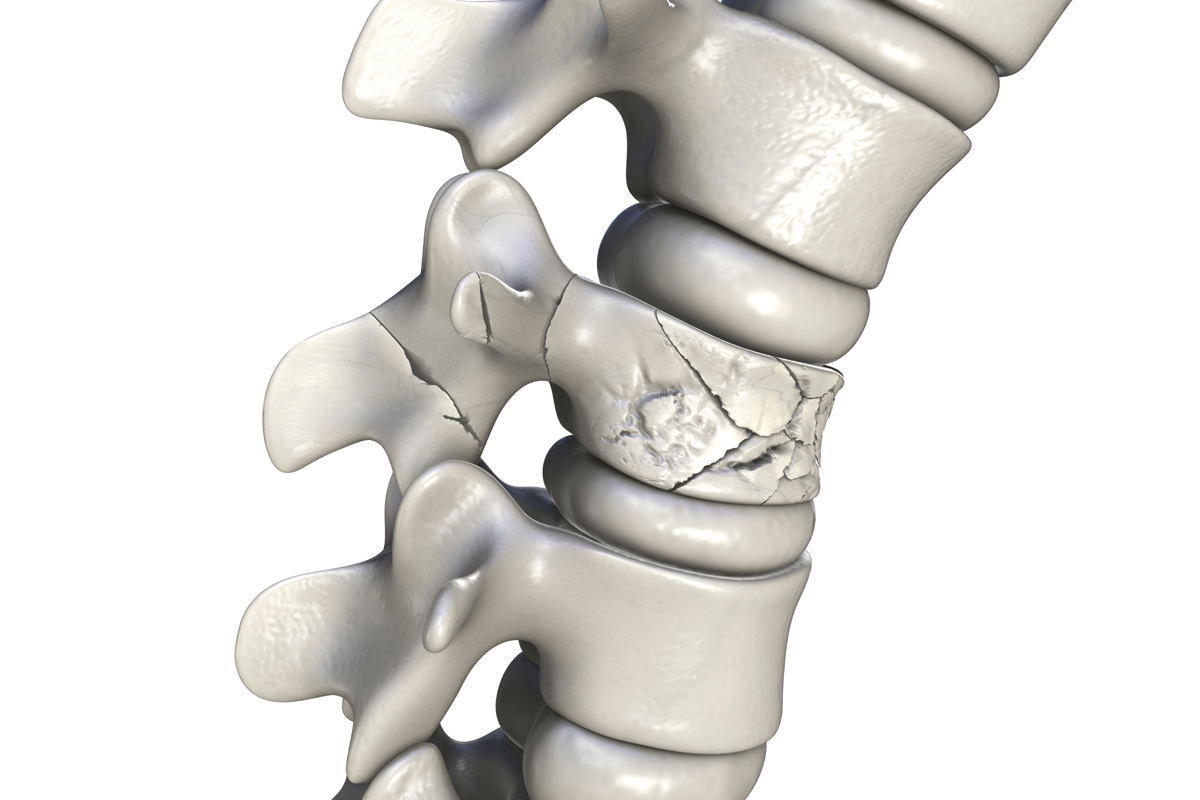
Given the demonstrated efficacy, cost-effectiveness, and relative safety of spinal decompression, it is important to explore the circumstances that necessitate this therapeutic intervention. The need for this procedure often arises in individuals suffering from chronic back pain caused by herniated or bulging discs, sciatica, degenerative disc disease, or spinal stenosis.
Decompression affordability plays a significant role in the decision-making process. The cost of spinal decompression can be high, particularly when multiple sessions are required. However, the overall cost-effectiveness is seen when considering the potential for reducing or eliminating the need for invasive surgeries and long-term medication use.
Insurance coverage is another critical aspect to consider. While not all insurance plans cover spinal decompression, many do recognize its potential benefits and provide partial or full coverage. It is important for patients to consult with their insurance providers to determine the extent of coverage and any out-of-pocket expenses they may incur.
How Spinal Decompression Works
To understand the mechanism of spinal decompression, it is essential to explore the intricacies of this therapeutic intervention, which primarily relies on the application of controlled, gradual, and precise traction to the spine. The decompression equipment creates a negative pressure or vacuum within the spinal disc, aiding the movement of oxygen, nutrients, and fluids into the disc to promote healing.
The following four steps elucidate the operational details of spinal decompression:
- The patient is positioned on a specially designed table connected to the decompression equipment, ensuring comfort and stability.
- Customized settings are configured into the system to apply specific, controlled traction to targeted spinal segments.
- The decompression equipment applies and releases traction alternately, creating a vacuum effect within the damaged disc, promoting retraction of the herniated or prolapsed disc material.
- The process is repeated over several sessions, with each session typically lasting between 30 to 45 minutes.
The effectiveness of spinal decompression is directly tied to the quality of decompression equipment and the expertise of the practitioner, both of which contribute to the overall decompression cost. The therapeutic efficacy, safety, and non-invasive nature of spinal decompression make it a viable treatment option for spinal disorders.
Types of Spinal Decompression Techniques
Understanding the variety of spinal decompression techniques can further elucidate the versatility and adaptability of this therapeutic approach to treating different spinal conditions. Two primary methods are surgical and nonsurgical decompression.
Surgical decompression, such as laminectomy or microdiscectomy, involves removing the source of pressure on the spinal cord or nerve roots, providing immediate relief. However, it carries inherent risks associated with invasive procedures and requires a significant recovery period.
Nonsurgical decompression, on the other hand, employs traction devices or techniques to gradually relieve spinal pressure. This approach is non-invasive, and while results may take longer to manifest, it carries fewer risks and requires minimal recovery time.
A decompression cost analysis must consider these factors. Surgical methods tend to be costlier upfront due to hospitalization, anesthesia, and postoperative care requirements. Nonsurgical alternatives often require multiple sessions, which, while individually less expensive, can accumulate over time.
Patient eligibility criteria for each technique differ. Surgical candidates often have severe, debilitating pain, neurological deficits, or conditions unresponsive to conservative treatments. Conversely, nonsurgical decompression is generally suitable for patients with mild to moderate symptoms, who have failed to respond to initial interventions like medication, physiotherapy, or injections.
Preparing for a Spinal Decompression Session
Patient preparation for a spinal decompression session, whether surgical or nonsurgical, involves a series of specific steps designed to optimize the treatment outcome and patient safety. This preparation requires both physical and emotional readiness, along with specific decompression diet suggestions.
- Physical Examination: A thorough physical examination helps determine the precise nature of the spinal problem. This includes imaging studies such as MRI or CT scans, and potentially nerve conduction studies.
- Decompression Diet Suggestions: A well-rounded diet is vital for faster recovery. Patients are advised to increase protein intake for muscle repair, consume adequate amounts of calcium and vitamin D for bone health, and maintain hydration.
- Emotional Readiness for Decompression: Emotional preparedness is as important as physical readiness. Patients should understand the procedure, its benefits, potential risks, and recovery process. Psychological preparation can significantly impact the overall treatment outcome.
- Preoperative Instructions: These may include stopping certain medications, fasting instructions, and arranging for post-procedure assistance.
The above-mentioned steps are fundamental in preparing for a spinal decompression session. These measures help guarantee the procedure’s success, minimize potential complications, and promote a quicker recovery.
The Spinal Decompression Procedure
Having adequately prepared for the procedure, we now turn our attention to the specifics of the spinal decompression process itself. Decompression efficacy is primarily dependent on the precise application of a controlled mechanical force to the spinal column, which is performed using a specially designed decompression table. The patient, positioned supine or prone depending on the vertebral level to be treated, is securely fastened to the table via a pelvic harness and chest support.
The decompression machine, programmed with patient-specific parameters, then applies a gentle pull to the spine, creating a negative intradiscal pressure. This leads to retraction or repositioning of the herniated or bulging disc material, and promotes the diffusion of water, oxygen, and nutrient-rich fluids into the disc, fostering a conducive environment for healing.
Patient eligibility for spinal decompression is determined by a thorough medical evaluation. Contraindications include pregnancy, advanced osteoporosis, spinal fusion, artificial disc replacements, and certain types of malignancies. However, for eligible patients suffering from conditions such as disc herniation, degenerative disc disease, and facet joint syndromes, spinal decompression can provide significant pain relief and improved function, reaffirming its efficacy as a non-invasive therapeutic option.
Post-Decompression Care and Recovery
Upon completion of the spinal decompression procedure, thorough attention shifts towards post-operative care and the recovery process, which plays a critical role in enhancing treatment outcomes and minimizing potential complications. Post-decompression care involves meticulous planning and preparation, with the prime aim of mitigating post-surgical pain, expediting the recovery process, and restoring the patient’s mobility.
Post-decompression care and recovery often involves a holistic approach, including:
- Pain Management: The use of analgesics and non-steroidal anti-inflammatory drugs might be initiated to reduce post-operative discomfort, promote healing, and improve patient satisfaction.
- Rehabilitation Exercises: Tailored physiotherapy and rehabilitation exercises are recommended to strengthen spinal muscles, enhance flexibility, and improve overall spine health.
- Patient Education: Patients are educated about the importance of maintaining proper posture, lifting techniques, and daily activities that can help prevent future spinal problems.
- Follow-up Assessments: Routine follow-ups are carried out to monitor the patient’s progress and to make adjustments in the treatment plan if necessary.

Pros and Cons of Spinal Decompression
As we move on to the topic of ‘Pros and Cons of Spinal Decompression,’ we will critically assess the advantages and potential risks associated with this procedure. The benefits of decompression will be examined, focusing on its efficacy in relieving spinal pressure and reducing pain. Concurrently, we will also highlight possible risks, providing a balanced perspective on this method of treatment.
Benefits of Decompression
In the domain of spinal health, the benefits and drawbacks of spinal decompression warrant an in-depth discussion, given its increasing prominence as a non-invasive therapeutic intervention.
- Decompression Cost Effectiveness: Spinal decompression is cost-effective compared to invasive surgical procedures. It eliminates the need for hospitalization, anesthesia, and post-operative care.
- Decompression for Athletes: Athletes experiencing back pain can benefit significantly from spinal decompression. It aids in rapid recovery, facilitates better physical performance, and minimizes the risk of re-injury.
- Non-Invasive: It is a non-surgical procedure, reducing the risks associated with invasive treatments.
- Pain Management: Spinal decompression alleviates chronic back pain by relieving pressure on spinal discs, thereby improving the patient’s quality of life.
Potential Decompression Risks
While spinal decompression presents multiple benefits, it is essential to also consider its potential risks, understanding that every medical procedure encompasses inherent uncertainties and possible side effects. Risk factors identification becomes paramount in ensuring patient safety. These risk factors may include age, overall health status, and the presence of any other diseases. Decompression contraindications should also be taken into account, including severe osteoporosis, obesity, or previous unsuccessful back surgeries. Potential risks may also involve temporary muscle spasms, skin irritation, and in rare cases, nerve damage or disc injury. It is critical that patients fully comprehend these risks before undertaking the procedure, and that healthcare providers have a thorough understanding of the patient’s health history to minimize potential complications.
Risks and Side Effects
While spinal decompression offers a non-surgical solution to chronic back pain, it is not without its potential risks and side effects. From minor discomfort to more serious complications, understanding these potential outcomes is essential to making an informed decision about treatment. The subsequent discussion will detail the potential risks, explore the side effects, and provide strategies for mitigating negative outcomes.
Understanding Decompression Risks
What potential risks and side effects might one encounter when undergoing spinal decompression therapy? Understanding these risks involves acknowledging potential decompression contraindications and engaging in risk management.
- Infection: This is a rare but serious risk. Sterile techniques are essential to mitigate this.
- Bleeding or Hematoma: Patients with bleeding disorders or on anticoagulants may be at higher risk.
- Neurological deterioration: Although extremely rare, it is possible for patients to experience neurological issues post-procedure.
- Worsening of symptoms: Some conditions, like extreme osteoporosis, may worsen after decompression treatment.
These potential risks underscore the necessity for thorough patient evaluation and risk-benefit analysis prior to proceeding with spinal decompression therapy. A careful approach guarantees patient safety and optimizes therapeutic outcomes.
Potential Side Effects
When evaluating the potential side effects of spinal decompression therapy, one must consider both the immediate aftermath of the procedure and long-term implications. Contrary to decompression therapy myths, side effects are typically minimal and temporary, including minor discomfort, muscle spasms, or slight skin irritation from the harness. However, more severe effects, such as nerve damage, disc injury, or worsening of existing conditions, are rare but should be acknowledged. Personalized decompression programs can minimize these risks by tailoring treatment to individual patient needs, taking into account factors such as age, health status, and the nature of the spinal issue. Informed patients and skilled practitioners working together can make spinal decompression a safe, effective treatment option.
Mitigating Negative Outcomes
In order to effectively mitigate the potential risks and side effects associated with spinal decompression therapy, a thorough approach to patient assessment, treatment planning, and post-procedure care is essential.
- Patient Assessment: A detailed patient history and physical examination should be conducted to identify any potential decompression complications.
- Treatment Planning: The treatment plan should be tailored to the patient’s unique condition and needs, taking into account the potential risks and benefits of spinal decompression.
- Procedure: The procedure itself should be performed by a trained and experienced medical professional to mitigate the risk of decompression complications.
- Post-procedure Care: After the procedure, patients should receive thorough follow-up care, including physical therapy if necessary, to promote healing and prevent complications.
Decompression cost considerations should also be discussed with the patient, to make sure they are fully aware of the financial implications.
Success Stories and Testimonials
Numerous patients have reported remarkable improvement in their condition following spinal decompression therapy, attributing their enhanced quality of life to this advanced, non-surgical intervention. These patient experiences showcase a positive trend in decompression outcomes, which is essential in understanding the efficacy of the procedure.
Notable accounts include patients who experienced chronic lower back pain for years, which drastically diminished following several sessions of spinal decompression. Another compelling testimony comes from a patient who, after suffering from a herniated disc, reported significant pain reduction and increased mobility post-treatment.
A detailed review of these testimonials indicates that patients generally experience an increased ability to perform daily activities without pain, heightened overall physical function, and a reduction in the need for pain medication. This evidence suggests that spinal decompression therapy has a significant positive impact on patients’ lives.
Importantly, these success stories are not isolated incidents. A multitude of testimonials point towards a consistent pattern of positive outcomes, reinforcing the credibility of spinal decompression therapy as a viable treatment option for certain spinal conditions. In conclusion, these patient experiences and decompression outcomes affirm the potential of this non-invasive therapy in managing and improving spinal health.
Alternatives to Spinal Decompression
While spinal decompression therapy has proven effective for many, it’s worth exploring alternative treatment options that may better suit the individual health circumstances and needs of certain patients.
- Physical Therapy: This non-surgical alternative focuses on enhancing mobility and relieving pain through exercises and manual therapy techniques.
- Decompression Diet Influence: Nutritional interventions can enhance the benefits of spinal decompression or serve as an alternative. A well-rounded diet, rich in anti-inflammatory foods, can help reduce pressure on the spine, promote healing, and improve overall spine health.
- Chiropractic Care: This involves the manual adjustment of the spine by a trained chiropractor to improve spinal function and alleviate discomfort.
- Medication: Certain drugs like non-steroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants can help manage symptoms.
These alternatives may be used independently or in conjunction with spinal decompression therapy, depending on the patient’s unique needs and health status. It’s crucial that patients engage in a thorough discussion with their healthcare provider to determine the most appropriate course of treatment.
Frequently Asked Questions
Can Spinal Decompression Help With Scoliosis?
Scoliosis progression can indeed be influenced by various interventions. Although decompression efficacy is not universally agreed upon, some studies suggest it may alleviate symptoms by reducing pressure on the spinal nerves and improving alignment.
Can I Exercise During a Spinal Decompression Treatment Course?
Certainly, exercise can be incorporated during a treatment course, but caution is necessary. Decompression precautions must be adhered to, and the types of exercises carried out should be gentle and approved by your healthcare provider.
What Is the Cost of a Typical Spinal Decompression Session?
The cost of a decompression session varies widely, ranging from $30 to $200 per session depending on location and provider. It’s crucial to weigh decompression risks and explore alternative treatments before finalizing a treatment plan.
Can I Return to Work Immediately After a Decompression Session?
Typically, return to work post-decompression depends on your job’s physical demands. Recovery time varies, but individuals can often resume light activities immediately. However, consult your healthcare provider for personalized advice on post decompression activities.
Is Spinal Decompression Covered by Most Health Insurance Policies?
The coverage of decompression eligibility varies among health insurance policies. It’s essential to verify with your individual provider to understand any insurance limitations concerning this specific procedure.