Spinal fractures, a critical health issue, often present a myriad of symptoms that may be overlooked due to their non-specific nature. These fractures can be caused by various factors, from traumatic injuries to diseases like osteoporosis. However, the real challenge lies in the early identification of these fractures to prevent potential long-term complications. As we progress, we will unravel the complexity of spinal fractures, their symptoms, and causes, offering insights into the importance of prompt diagnosis and effective treatment. The question then becomes, how well do we understand and recognize these signs?
Understanding Spinal Fractures
Spinal fractures, a severe medical condition often resulting from trauma or disease, involve a break in the continuity of the spinal bone, leading to potential complications and significant impact on an individual’s quality of life. This type of fracture can be particularly debilitating, as it affects the vertebrae, the vital bones that make up the spine. Damage or disruption to these structures can impede the spinal cord’s function, leading to varying degrees of physical disability.
Fracture rehabilitation plays a pivotal role in the recovery process, helping to restore functionality and reduce pain. It typically involves a multidisciplinary approach, incorporating physiotherapy, pain management and, in some cases, surgical intervention. Patient education is also an integral part of the rehabilitation process, empowering individuals with the knowledge to manage their condition effectively.
Spinal anatomy anomalies can predispose individuals to spinal fractures. These might include congenital defects, degenerative changes due to aging, or abnormalities developed due to lifestyle factors or other health conditions. Understanding these anomalies is crucial to both preventive measures and appropriate treatment strategies, guiding the clinical decision-making process to optimise patient outcomes.
Anatomy of the Spine
To fully comprehend the complex nature of spinal fractures, it’s imperative to delve into the intricate anatomy of the spine, a robust structure that houses and safeguards the body’s central nervous system. The spine, also known as the vertebral column, is a stack of 33 individual bones, called vertebrae, which are divided into five distinct regions.
- Cervical Spine: The neck region, containing seven vertebrae that provide support and flexibility for the head.
- Thoracic Spine: The chest region, consisting of twelve vertebrae that anchor the ribs.
- Lumbar Spine: The lower back region, composed of five large vertebrae that bear the majority of the body’s weight.
The vertebral function extends beyond structural support. Each vertebra encases the spinal cord, a critical pathway for transmitting signals between the brain and the rest of the body. Between each vertebra are intervertebral discs, which contribute to spine flexibility and act as shock absorbers during movement.
Understanding the anatomy of the spine is crucial because disturbances in any part of this complex structure can lead to severe complications, such as spinal fractures.
Different Types of Spinal Fractures
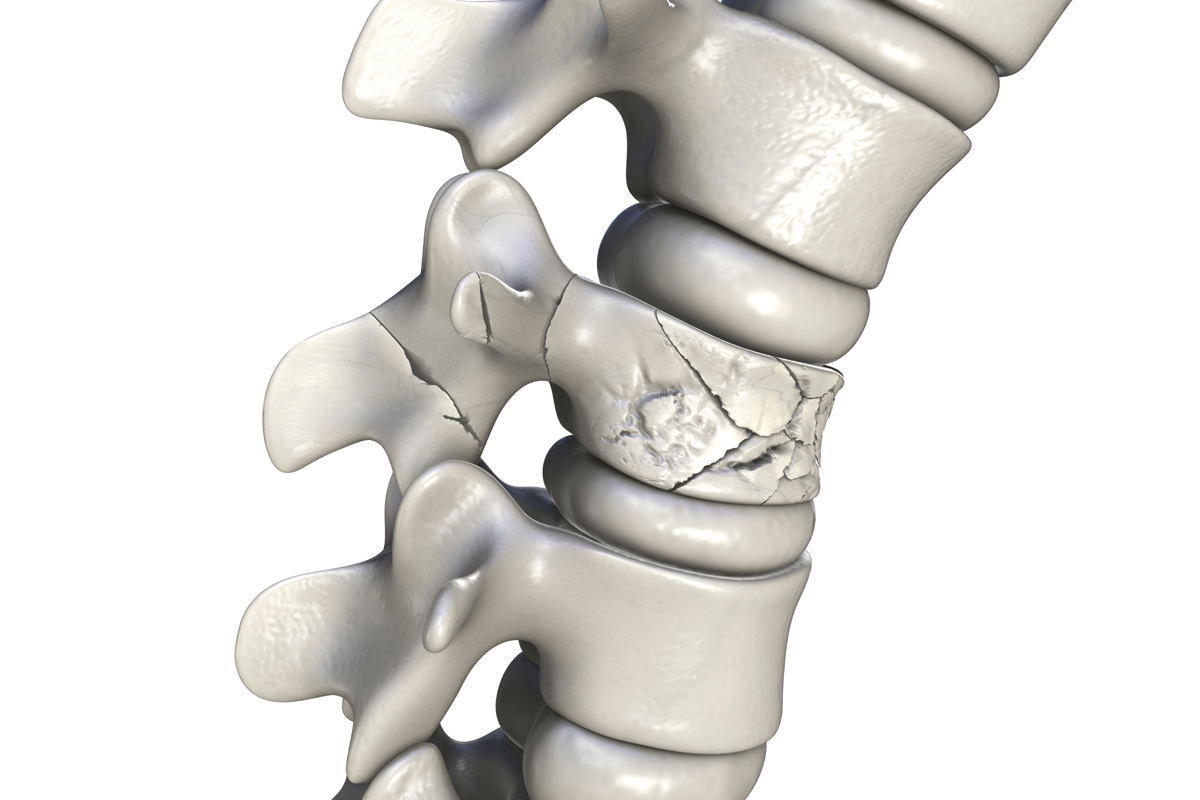
There are several distinct types of spinal fractures, each presenting unique challenges in terms of diagnosis and treatment. These fractures differ not only in their location along the spinal column, but also in the nature of the injury and the specific causes behind their onset. Understanding the characteristics of these fractures is critical to their effective management and eventual resolution.
Common Spinal Fracture Types
In the realm of orthopedic medicine, several distinct types of spinal fractures are recognized, each with unique causes, symptoms, and treatment strategies. Overcoming fracture misconceptions is critical to understanding these types and addressing the associated rehabilitation challenges.
- Compression Fractures: Often resulting from osteoporosis, these fractures occur when the bone in the spine collapses, causing pain and decreased height.
- Axial Burst Fractures: These are characterized by the dispersion of the vertebra in multiple directions due to extreme pressure, often caused by falls from considerable heights.
- Flexion/Distraction Fractures: Also known as ‘seatbelt fractures’, these are caused by abrupt forward movement, typically seen in vehicular accidents.
Each of these fractures presents unique challenges, requiring tailored treatment and rehabilitation strategies to ensure optimal patient recovery.
Causes of Spinal Fractures
Various factors contribute to the occurrence of different types of spinal fractures, ranging from degenerative diseases like osteoporosis to traumatic incidents such as falls and vehicular accidents. Spinal infection risks are also significant contributors. Bacterial or fungal infections can cause spinal fractures by weakening the bone structure. Genetic predispositions, including conditions like Ehlers-Danlos syndrome and Marfan syndrome, can also lead to spinal fractures. These conditions affect the body’s connective tissue, making the spine more susceptible to fractures. Certain lifestyle choices, such as tobacco use and excessive alcohol consumption, can also increase the risk of spinal fractures by decreasing bone density. Understanding these causes is key in preventing spinal fractures and managing existing ones.
Common Causes of Spinal Fractures
Spinal fractures predominantly occur due to three principal causes, namely trauma, osteoporosis, and tumors. Trauma-induced spinal fractures are commonly associated with high-impact incidents such as motor vehicle accidents or falls. Conversely, osteoporosis and certain types of tumors can weaken spinal integrity, increasing susceptibility to fractures even under minimal stress.
Trauma-Induced Spinal Fractures
Among the most common causes of spinal fractures, trauma-induced incidents take a significant lead, often resulting from severe accidents, falls, or sports injuries. These traumatic events can cause a sudden, forceful impact on the spine, leading to fractures. The fracture healing process in such cases is often complex and lengthy, requiring intensive medical intervention and physiotherapy.
Three key areas impacted by trauma-induced spinal fractures are:
1. Physical Health: Severe pain, limited mobility, and long-term disability can result.
2. Psychological Health: Patients often face anxiety, depression or post-traumatic stress disorder.
3. Quality of Life: The combined physical and psychological impacts drastically affect daily living activities and social interactions.
Addressing these areas holistically is essential for comprehensive patient care and recovery.
Osteoporosis and Spine Fractures
In addition to trauma-induced incidents, osteoporosis is a prevalent cause of spinal fractures, significantly contributing to the global burden of these debilitating injuries. This disease results in decreased bone density, leading to a heightened risk of fractures. The Bone Density Correlation with spinal fractures is evident in osteoporosis patients, as the porous nature of their bones makes them weak and susceptible to breaks. Furthermore, Lifestyle Impact plays a crucial role in osteoporotic spinal fractures. Factors such as sedentary behavior, poor nutrition, smoking, and excessive alcohol use can exacerbate bone loss, thereby enhancing the susceptibility to fractures. Thus, osteoporosis remains a critical focus in the prevention and management of spinal fractures.
Tumors Causing Spinal Fractures
Did you know that, apart from osteoporosis and trauma, tumors are another common cause of spinal fractures? Tumors, both benign and malignant, can weaken the vertebral column, making it susceptible to fractures.
There are primarily three tumor types associated with spinal fractures:
- Metastatic tumors: These are the most common spinal tumors that originate from cancer in another part of the body and spread to the spine.
- Primary bone tumors: Though rare, these originate in the spine itself.
- Multiple myeloma: This type of cancer affects the bone marrow and can cause multiple fractures in the spine.
Spinal tumor prognosis depends on several factors, including the type of tumor, its size, location, and the overall health of the patient. Early detection and treatment can significantly improve outcomes.

High-Risk Groups for Spinal Fractures
Certain demographic groups are more susceptible to spinal fractures due to factors such as age, gender, and underlying health conditions. Lifestyle factors and genetic predispositions also play a significant role in determining high-risk groups.
The aging population, particularly women post-menopause, is high-risk due to the natural bone density loss that occurs with age, exacerbated by conditions like osteoporosis. Individuals with certain genetic predispositions, including specific types of collagen disorders, are also at a higher risk of developing spinal fractures.
Lifestyle factors such as lack of physical activity, poor nutrition, or habits like smoking and alcohol can contribute to reduced bone density and thus, amplify the risk of fractures. In addition, people who have undergone spinal surgeries or have chronic conditions such as arthritis or cancer, are at an elevated risk for spinal fractures.
Certain professions or activities that involve heavy lifting, repetitive motion, or a high risk of trauma, such as construction workers or athletes, are also more likely to experience spinal fractures. Understanding these risk factors is crucial for both prevention and early detection of spinal fractures.
Recognizing Spinal Fracture Symptoms
Recognizing the symptoms of spinal fractures is crucial for early detection and effective treatment. We will examine the common symptoms and discuss the patterns of pain typically associated with these types of injuries. This discussion will provide a more comprehensive understanding of the indicators of spinal fractures.
Identifying Common Symptoms
Patients with spinal fractures often present a range of specific symptoms that indicate the severity and location of the injury. These symptoms can sometimes lead to misdiagnosis, due to their similarity with other conditions, causing a psychological impact on the patient.
Common symptoms include:
1. Severe and sudden back pain: This may be localized to the fracture site or it can radiate to other parts of the body.
2. Limited mobility: Patients may experience difficulty in walking or moving.
3. Height loss or deformity of the spine: These are physical manifestations of a severe spinal fracture.
Understanding these symptoms is crucial for accurate diagnosis and effective treatment planning. Nevertheless, symptom misdiagnosis can delay necessary treatment, escalating the psychological impact on patients.
Understanding Pain Patterns
To understand spinal fracture symptoms more effectively, it is imperative to delve into the varying pain patterns that could indicate this severe type of injury. Pain may be immediate or delayed, localized or radiating, and could vary in severity from mild discomfort to debilitating agony. Pain management techniques are crucial in dealing with these symptoms, often involving a combination of medications, physical therapy, and sometimes surgical intervention.
A key aspect of patient care involves the psychological impact assessment. Chronic pain can lead to emotional distress, including anxiety and depression, which in turn can exacerbate the perception of pain. Therefore, a holistic approach to pain management, incorporating both physical and psychological therapies, can significantly improve the quality of life for patients suffering from spinal fractures.
Pain Indicators of Spinal Fractures
In understanding spinal fractures, it is crucial to identify the key pain indicators associated with this condition. Early detection can expedite fracture management and the implementation of effective rehabilitation strategies.
- Persistent Back or Neck Pain: This is often the most noticeable symptom of a spinal fracture. The pain may be sharp or dull, continuous or intermittent, localized or diffused. It may increase with movement and decrease when resting.
- Pain that Radiates: The pain might not be confined to the back or neck. It could also radiate to the arms or legs, similar to nerve pain. This is usually due to the compression of spinal nerves caused by the fracture.
- Increased Pain with Standing or Walking: The act of standing or walking can put additional stress on the injured spine, intensifying the pain. Conversely, lying down may provide some relief.
These pain indicators are critical in the initial diagnosis of spinal fractures. Nevertheless, their presence does not confirm a spine fracture. Additional diagnostic procedures, such as imaging studies, are necessary to confirm the diagnosis and to guide treatment planning.
Non-Pain Symptoms of Spinal Fractures
Beyond the realm of pain, spinal fractures can manifest a variety of non-pain symptoms that are equally crucial for diagnosis and treatment planning. These symptoms often provide critical insight into the severity of the fracture, its potential complications, and the most appropriate therapeutic approach.
One common non-pain symptom is a noticeable change in posture or spinal alignment, which may manifest as kyphosis (a forward curvature of the spine) or scoliosis (a sideways curvature). A fracture can also lead to reduced sensation or numbness in the limbs, or even paralysis in severe cases.
These physical changes often have a significant emotional impact. Patients may experience feelings of anxiety, depression, and fear due to the uncertainty of their condition and potential disability. These emotional responses can further complicate the overall health status and should be addressed during the course of treatment.
Moreover, patients may present with gastrointestinal or genitourinary symptoms as fracture complications. These include constipation, incontinence, or difficulty in urination, which are indicative of the involvement of spinal nerves controlling these functions.

How Spinal Fractures Affect Mobility
Given the profound impact of spinal fractures on the body’s function and alignment, the implications for patient mobility are a significant area of concern. Spinal fractures can lead to several mobility limitations, not only because of the pain and discomfort but also due to the physical restrictions they impose.
- Restricted Range of Motion: Spinal fractures can limit the range of motion in the back, making it difficult to bend or twist. This restriction can affect simple activities such as picking up items, getting dressed, or even walking.
- Decreased Strength and Stability: The muscles around the spine may weaken due to the fracture, reducing the patient’s overall strength and stability. This weakness can lead to frequent falls, further exacerbating the injury.
- Prolonged Bed Rest: Extended periods of immobility after a spinal fracture can lead to muscle atrophy and joint stiffness, worsening the mobility issues.
Fracture rehabilitation plays a crucial role in patient recovery, with the use of mobility aids often being a necessary part of the process. Physical therapy, exercises, and assistive devices like walkers or wheelchairs can help patients regain their mobility and independence, promoting a better quality of life post-injury.
Diagnostic Procedures for Spinal Fractures
Several comprehensive diagnostic procedures are employed in the accurate identification and assessment of spinal fractures. Primarily, these procedures aim to evaluate the severity of the fracture and determine the most effective rehabilitation strategies.
Physical examinations are typically the first step in the diagnostic process. This involves a thorough evaluation of the patient’s medical history, a detailed examination of the spine, and the assessment of neurological signs such as pain, weakness, numbness, or changes in reflexes.
Radiographic examinations, including X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI), offer a more detailed view of the spinal structure. X-rays can show the location and extent of the fracture, while CT scans provide a more detailed image of the bone and surrounding tissues. MRI scans are particularly useful in identifying any damage to the spinal cord and nerves.
In some cases, a bone scan may be necessary to monitor the fracture healing process. This involves injecting a small amount of radioactive material into the bloodstream, which then accumulates in the bones and can be detected by a scanner.
These diagnostic tools, together with a comprehensive clinical evaluation, provide a detailed understanding of the injury and inform the development of effective treatment and rehabilitation strategies.
Treating Spinal Fractures
The treatment of spinal fractures necessitates a multifaceted approach, often encompassing both non-surgical and surgical interventions, tailored specifically to the patient’s individual diagnosis and overall health status. The primary aim of these interventions is to manage pain, prevent further spinal deformity, and restore as much function as possible.
- Non-Surgical Interventions: Initially, most spinal fractures are treated conservatively. This includes bed rest, pain management with medications, and the use of braces to restrict movement and provide spinal stability.
- Surgical Interventions: If the fracture is severe or non-surgical interventions are ineffective, surgery may be necessary. Depending on the type of fracture and its location, different surgical procedures like vertebroplasty, kyphoplasty, or spinal fusion can be performed.
- Rehabilitation Strategies: Post-treatment, rehabilitation strategies play a crucial role in helping patients regain strength and enhance their quality of life. This may include physiotherapy, occupational therapy, and pain management programs.
The choice between non-surgical and surgical interventions depends on several factors, such as the severity and type of fracture, the patient’s age and overall health, and the presence of other medical conditions. A comprehensive, individualized treatment plan can help ensure the best possible outcome for patients with spinal fractures.
Preventing Spinal Fractures
Understanding how to prevent spinal fractures involves adopting lifestyle modifications, engaging in regular physical activity to strengthen the spine, and taking precautions to avoid accidents and injuries that can compromise spinal integrity. The first line of defense is fracture nutrition, which emphasizes consuming a diet rich in calcium and vitamin D to promote bone health and density. Supplementing with these nutrients, if dietary intake is insufficient, can be beneficial.
Posture training is another crucial preventive measure. Proper alignment of the spine during sitting, standing, and lifting minimizes the strain on the spinal column, reducing the risk of injury. Ergonomic adjustments to furniture and workstations can also aid in maintaining good posture throughout the day. Specific exercises designed to enhance core strength and flexibility also contribute to spinal stability.
Precautionary measures like wearing seat belts in vehicles and using safety equipment during high-risk activities can protect the spine from traumatic injury. Regular check-ups to monitor bone health, especially in the elderly and those with risk factors for osteoporosis, are also essential.
Frequently Asked Questions
What Is the Recovery Time for Various Types of Spinal Fractures?
Recovery time for spinal fractures varies depending on the fracture type, patient’s overall health, and the effectiveness of pain management strategies and fracture prevention measures. Typically, it ranges from several weeks to a few months.
Are There Specific Exercises or Physical Therapy Routines That Can Help in the Recovery Process After a Spinal Fracture?
Yes, certain exercises and physical therapy routines can aid recovery post spinal fracture. Pain management techniques and mobility improvement methods, including stretching and strength training, can help restore function and reduce discomfort during the healing process.
How Can a Spinal Fracture Affect Mental Health?
Spinal fractures often lead to emotional trauma due to sudden lifestyle changes. The physical limitations can necessitate significant psychological adjustments, potentially inducing stress, anxiety, or depression, thereby impacting the individual’s overall mental health.
What Are Some Potential Complications or Side Effects of Spinal Fracture Treatments?
Potential complications of spinal fracture treatments can include infection, nerve damage, and ongoing pain. Treatment costs can become significant, especially for long-term care, and may not be fully covered by insurance policies.
Can Diet or Nutrition Play a Role in the Recovery Process After a Spinal Fracture?
Yes, diet and nutrition significantly influence recovery post spinal fracture. Nutritional supplements benefits include enhanced bone healing, while adequate hydration impacts overall health and healing. A balanced diet is crucial for optimal recovery.