The process of diagnosing spine injuries is a complex yet fascinating area of medical practice, employing a blend of patient interaction, physical examination techniques, and advanced imaging technologies. The collection of patient history provides context to the injury, while physical examinations offer immediate insights into the state of the spine and nerve function. Supplementing these are advanced diagnostic imaging procedures, which serve to illuminate the intricate structure of the spine in vivid detail, thereby aiding in precise injury identification. However, one must ask, how do these methods work in concert to provide an accurate diagnosis, and what are their individual strengths and limitations?
Understanding Spine Injuries
Exploring the intricate world of spine injuries, it is essential to comprehend that these can range from mild strains to severe traumatic events, each with its unique pathophysiology and implications for patient care. A deep understanding of spinal cord anatomy is paramount to adequately diagnose and treat these conditions. Comprised of 31 pairs of nerves, the spinal cord extends from the brainstem to the lower back, acting as a conduit for sensory and motor functions.
Spine injuries can profoundly impact this complex system, disrupting the communication between the brain and body, leading to a range of symptoms from pain to paralysis. Hence, early detection and intervention are critical in minimizing potential damage and optimizing patient outcomes.
Injury prevention strategies play an important role in the overall management of spine health. Encouraging regular exercise, promoting proper ergonomics, and advocating for safety in sporting and occupational environments are key aspects of these strategies. By instilling these preventive measures, we can notably reduce the incidence of spinal injuries, ultimately enhancing overall patient health and quality of life. Understanding spine injuries is the first critical step to effective diagnosis, treatment, and prevention.
Initial Consultation Process
Commencing with the initial consultation process, a thorough and systematic patient assessment is essential in the accurate diagnosis of spinal injuries. This is where the clinician can elicit valuable information that may guide the diagnosis and subsequent treatment plan.
The importance of patient history cannot be overstated. It provides the clinician with a detailed picture of the patient’s overall health status, lifestyle, and the onset and progression of the current spinal problem. This could include information about previous injuries, chronic conditions, or family history of spinal problems.
During the consultation, the healthcare provider should also guarantee consultation confidentiality. This not only respects the patient’s privacy rights, but also encourages the patient to share more openly about their symptoms and concerns.
To summarize, the initial consultation process should:
* Elicit a detailed patient history to understand the onset and progression of the spinal issue
* Guarantee consultation confidentiality to respect the patient’s privacy and promote open communication
* Use the collected information to guide the subsequent diagnostic and treatment plan
This essential first step sets the foundation for the rest of the diagnostic process, paving the way for more targeted physical examination techniques.
Physical Examination Techniques
In diagnosing spine injuries, physical examination techniques play a vital role. These techniques encompass initial observation methods, neurological assessments, and musculoskeletal evaluation techniques. A detailed understanding of these procedures can greatly enhance the accuracy of the diagnosis and treatment plan.
Initial Observation Methods
To accurately diagnose spine injuries, medical professionals often resort to a series of initial observation methods, which primarily involve carefully executed physical examination techniques. Effective patient communication is essential at this stage, as it allows the medical team to gain insights into the patient’s medical history, symptoms, and the nature of the injury.
In an emergency response situation, these quick assessments can be instrumental in determining the severity of the injury and initiating the most appropriate treatment. Some of the commonly used initial observation methods include:
- Inspection and palpation: Observing and feeling the spine for deformities or tenderness.
- Range of motion tests: Checking the patient’s ability to move in specific directions without pain.
- Special tests: These are specific movements or positions that can provoke symptoms and provide valuable diagnostic information.
Neurological Assessments
Delving deeper into the domain of physical examination techniques, neurological assessments play a pivotal role in diagnosing spine injuries as they provide essential information about the patient’s nerve function and potential damage. One common method applied is spinal reflex testing, which evaluates the integrity of specific nerve roots, thereby revealing any abnormalities. This test involves the use of a reflex hammer to stimulate a tendon and record the muscle’s response, providing vital data about the functioning of the respective nerves. Another technique used is pain threshold evaluation. This procedure gauges the patient’s tolerance to pain by applying varying degrees of pressure or temperature stimuli. These evaluations, coupled with the patient’s history and presenting symptoms, deliver a thorough understanding of the nerve-related aspects of a spine injury.
Musculoskeletal Evaluation Techniques
Shifting focus to musculoskeletal evaluation techniques, these physical examination methods are essential in providing thorough insights into the structural integrity and functional status of the patient’s spine.
These techniques often include:
- Spinal palpation, an evaluation method that relies heavily on the accuracy of the clinician’s touch. The spinal palpation accuracy in identifying vertebral deformities or irregularities is important in the diagnostic process.
- Musculoskeletal ultrasound, a non-invasive imaging technique that has gained utility in the assessment of muscles, ligaments, and other soft tissues surrounding the spine.
- Range of motion tests, which assess the spine’s flexibility and any limitations due to pain or stiffness.
These techniques, combined with patient history and other diagnostic methods, help provide a thorough assessment of potential spine issues.
Overview of Diagnostic Imaging
In the domain of spine injuries, diagnostic imaging plays an integral role in facilitating accurate diagnoses. Two key modalities, Radiographic Assessments and Magnetic Resonance Imaging (MRI), are essential tools for clinicians in revealing the nature and extent of spinal injuries. These imaging techniques offer invaluable insights into the structural integrity of the spine, paving the way for targeted treatment strategies.
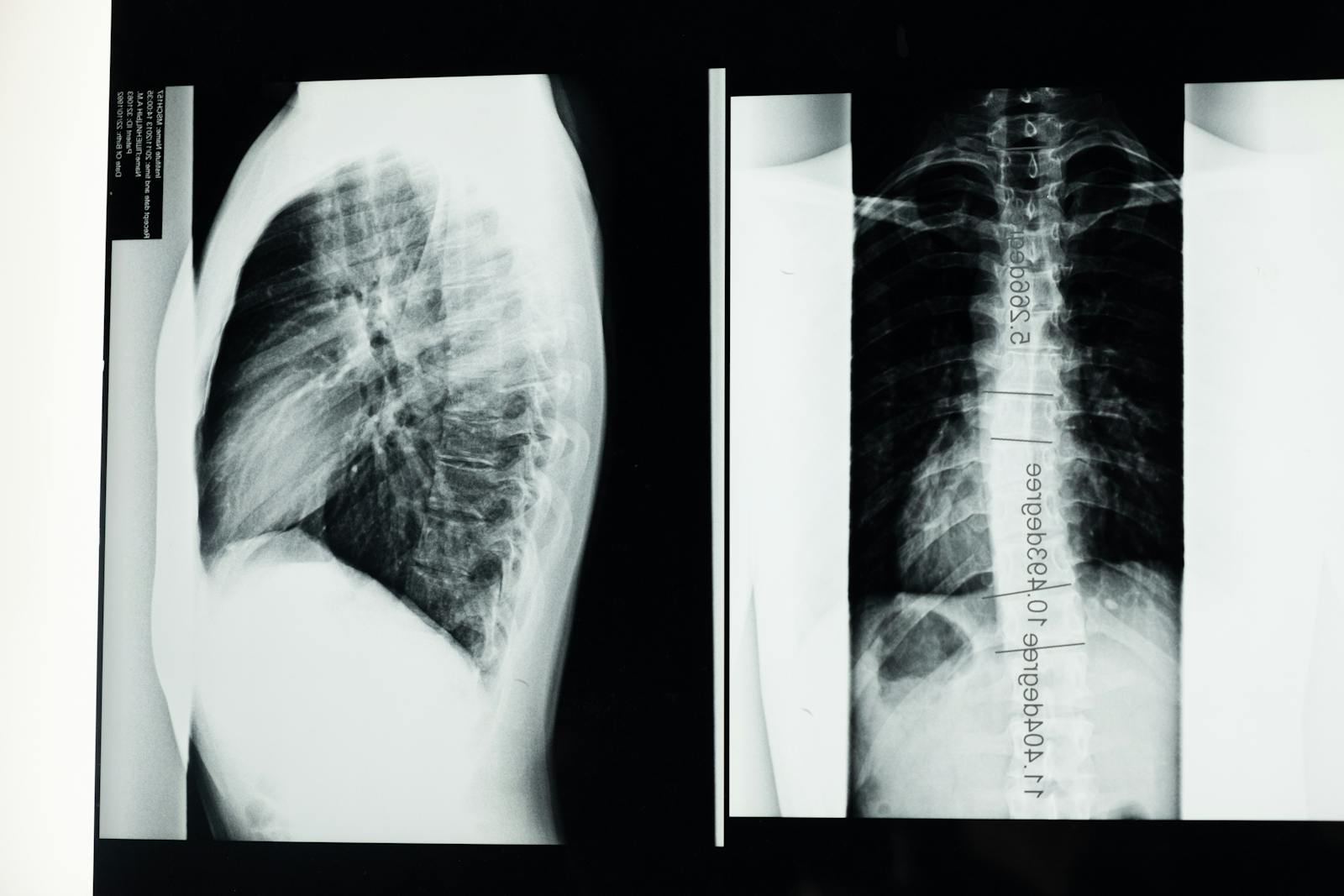
Understanding Radiographic Assessments
Frequently utilized in the evaluation of spine injuries, radiographic assessments provide an invaluable, detailed insight into the structure and condition of the spinal anatomy. However, these assessments aren’t without their limitations. While they offer excellent skeletal visualization, they can struggle to reveal soft tissue injuries or subtle abnormalities.
To overcome these radiographic limitations, contrast agents are often utilized. These substances, injected or swallowed by the patient, enhance the visibility of specific areas, helping clinicians to discern more details and make accurate diagnoses.
Key points to remember about radiographic assessments include:
- They provide detailed images of the spine
- Radiographic limitations may require the use of contrast agents for clearer imaging
- Contrast agents can enhance visibility of soft tissues or subtle abnormalities
MRI: Unveiling Spinal Injuries
While radiographic assessments play a crucial role in the initial evaluation of spinal injuries, Magnetic Resonance Imaging (MRI) offers a more thorough view, particularly when investigating soft tissue damage and subtle abnormalities. MRI’s superior imaging capability enables clinicians to identify and evaluate the severity of spinal injuries with remarkable precision. Recent Spinal MRI Innovations further enhance its diagnostic acumen, providing detailed 3D images of the spinal anatomy, including the spinal cord, vertebrae, and surrounding structures. Additionally, MRI Safety Measures, such as screening for metallic objects and monitoring of patients during the procedure, guarantee that the diagnostic process is safe and risk-free. Therefore, the MRI is an invaluable tool in the diagnostic landscape of spinal injuries, contributing significantly to accurate diagnosis and effective treatment.
X-rays for Spine Diagnostics
Delving into the field of spine diagnostics, X-rays serve as a fundamental tool, providing detailed images of the spinal structure and enabling professionals to identify any abnormalities or injuries. In the context of radiation safety, the risk of exposure during an X-ray procedure is relatively low, and advancements in X-ray technology have further minimized this risk while enhancing image quality.
X-rays for spinal diagnostics offer several advantages:
- They provide a thorough overview of the spine, allowing for the detection of fractures, tumors, and spinal deformities.
- Technological advancements in X-rays have enabled the production of high-resolution images, leading to more accurate diagnoses.
- X-rays are a cost-effective diagnostic tool, making them accessible to a broad range of patients.
In addition, X-ray images allow for the evaluation of bone density, which can be essential in diagnosing conditions such as osteoporosis. Although X-rays play a pivotal role in spinal diagnostics, they are often used in conjunction with other imaging techniques to provide a holistic view of the spine’s condition. The detailed nature of this diagnostic approach ensures a thorough understanding of the patient’s spinal health, leading to more effective treatment plans.
The Role of CT Scans
In addition to X-rays, Computed Tomography (CT) scans play an essential role in the thorough diagnosis and analysis of spinal injuries. CT scans provide a more detailed view of the spine than traditional X-rays, offering an accurate depiction of the bone structure and revealing any fractures or other abnormalities that may not be visible on an X-ray. The CT scan accuracy is particularly beneficial in acute trauma situations, where a thorough understanding of the injury is important for determining the most effective treatment plan.
However, along with its advantages, there are Radiation Exposure Concerns associated with CT scans. The level of radiation a patient is exposed to during a CT scan is significantly higher than during standard X-rays. While the risk associated with a single scan is typically low, repeated exposure could potentially increase the probability of developing cancer later in life. Hence, the use of CT scans should always be considered carefully, weighing the diagnostic benefits against the potential risks.
MRI: A Comprehensive Tool
Despite the potential radiation risks associated with CT scans, Magnetic Resonance Imaging (MRI) emerges as a thorough tool in diagnosing spinal injuries, offering detailed imaging without exposure to ionizing radiation. This sophisticated technology uses a powerful magnetic field, radio waves, and a computer to produce detailed pictures of the spine’s intricate structure, including bones, discs, and the surrounding soft tissues.
The use of MRI in spinal injury diagnosis comes with multiple benefits:
- It offers detailed images of the spine in multiple planes without any need for patient repositioning.
- Unlike X-rays and CT scans, MRI does not use ionizing radiation, making it safer for patients, particularly those who require multiple scans.
- It is excellent in visualizing soft tissue injuries, including those to the spinal cord and nerve roots.
However, the procedure is not without its precautions. MRI safety precautions are essential to prevent potential risks. For example, patients with certain implants or metallic objects in their bodies may not be suitable candidates for an MRI. Moreover, the use of contrast agents is common in MRI scans to improve visualization of certain tissues or blood vessels. Careful usage of these agents is vital to avoid allergic reactions or kidney problems. To summarize, MRI proves to be a thorough tool in diagnosing spinal injuries, prioritizing patient safety and precise imaging.
Discography in Spine Diagnosis
Shifting our focus to another diagnostic tool, discography provides valuable insight into the health of the spine’s discs, particularly in cases where other imaging modalities have not clarified the source of pain. This procedure involves injecting a contrast dye into the disc and observing its dispersion via fluoroscopic guidance.
Discography is particularly useful in identifying degenerative disc disease and disc herniation. However, like any invasive procedure, it’s not without potential complications. Discography complications can include infection, bleeding, nerve damage, and in rare cases, discitis – an inflammation of the intervertebral discs. Adequate patient preparation for discography is required to mitigate these risks.
Discography patient preparation involves a thorough medical history review and a physical examination to identify any contraindications. Patients are advised to avoid eating or drinking several hours before the procedure. In addition, certain medications may need to be discontinued.
Despite these precautions, discography should be reserved for situations where the source of a patient’s pain remains elusive after exhausting other non-invasive diagnostic modalities. With its potential risks and benefits, discography is a valuable tool in the diagnostic arsenal for spinal pathologies.

Myelography and Its Utility
Moving from discography, another significant tool in diagnosing spinal injuries is myelography, an imaging technique used to evaluate abnormalities of the spinal cord, nerve roots, and spinal lining. The procedure involves injecting a contrast dye into the spinal column, which then circulates around the spinal cord and nerve roots. X-ray or CT imaging is then used to reveal any abnormalities or injuries.
Myelography has several key advantages:
– It can provide detailed images of the spinal cord and nerve roots, even in regions that are difficult to reach with other imaging techniques.
– It can be combined with other imaging techniques like CT scans for more thorough results.
– Advancements in myelography have improved image quality and reduced the risk of complications.
Despite its utility, the procedure does have potential complications. Myelography complications can include allergic reactions to the contrast dye, infection, bleeding, and discomfort at the injection site. However, these risks are generally low, and the procedure is considered safe and effective for diagnosing a wide range of spinal conditions.
Exploring Electromyograms (EMGs)
As we continue our exploration of diagnostic techniques for spine injuries, it is essential to examine Electromyograms (EMGs). Primarily, we will be focusing on the procedural aspects of EMGs, the interpretation of test results, and potential risks and limitations associated with this method. Understanding these facets is vital for any healthcare professional involved in diagnosing and managing patients with spinal conditions.
Understanding Electromyograms Procedure
The electromyogram procedure, a cornerstone in diagnosing spinal injuries, is a sophisticated medical test that measures the electrical activity of muscles at rest and during contraction.
Key elements of this process include:
- EMG Patient Preparation: Prior to the procedure, patients are instructed to avoid caffeinated drinks and lotions. They are also advised to wear loose, comfortable clothing for easy electrode placement.
- Procedure Execution: Small, thin needles are inserted into the muscle to record electrical activity. The data collected helps physicians identify any neuromuscular abnormalities.
- EMG’s Historical Evolution: Since its inception in the late 19th century, EMG has continually evolved with technological advancements, improving its accuracy and reducing patient discomfort.
Understanding this procedure is essential for patients and medical professionals alike, enabling prompt and accurate diagnosis of spinal injuries.
Interpretation of EMG Results
Decoding the results of an Electromyogram demands profound expertise, as it involves careful scrutiny of the electrical activity patterns in muscles, both at rest and during contraction, to pinpoint any neuromuscular abnormalities. EMG interpretation challenges include differentiating between normal and abnormal patterns, distinguishing between primary muscle disease and neurogenic disorders, and understanding the implications of spontaneous activity.
Despite these challenges, the clinical significance of EMGs cannot be overstated. This diagnostic tool provides invaluable insights into the function and health of the muscles and nerves. It is particularly effective in identifying nerve damage resulting from conditions such as herniated discs, spinal stenosis, or degenerative disc disease. Ultimately, precise interpretation of EMG results is a crucial component in the thorough assessment of spine injuries.
EMGs: Risks and Limitations
While Electromyograms prove to be highly important in diagnosing various neuromuscular disorders and spine injuries, it is essential to take into account their potential risks and limitations.
- Risks: EMGs can occasionally cause mild discomfort, bleeding, or infection at the needle insertion site. Also, patients with bleeding disorders or those taking anticoagulants may face increased risks.
- Limitations: EMGs may not always definitively diagnose a condition, necessitating the use of EMG alternatives like Magnetic Resonance Imaging (MRI) or Computerized Tomography (CT) scans.
- Advancements: Despite limitations, EMG advancements have expanded its capabilities, improving accuracy and patient comfort.
Always consider these factors alongside the potential benefits when deciding on whether to use EMGs for diagnosing spine injuries.
Nerve Conduction Studies Explained
In the field of spine injury diagnosis, Nerve Conduction Studies (NCS) play an essential role, offering detailed insights into the health and functioning of the patient’s peripheral nerves. These studies provide a crucial, highly accurate method for detecting nerve damage, aiding in nerve damage prevention and enabling healthcare providers to devise effective treatment plans.
NCS involves stimulating nerves at various points using small electric shocks and measuring the speed and intensity of the resulting nerve impulses. This data reveals any anomalies in nerve function, such as slowed conduction, indicating possible nerve damage. Therefore, NCS can diagnose conditions like nerve compression disorders, nerve injuries, and peripheral neuropathies, which are often associated with spine injuries.
Recent conduction study advancements have improved the precision and accuracy of NCS. Technological innovations, such as digital signal processing and advanced electrode designs, have enhanced the resolution and sensitivity of the tests, allowing for more nuanced readings. These advancements have greatly enhanced the diagnostic capabilities of NCS, making it a cornerstone of modern neurodiagnostic medicine and a crucial tool in the diagnosis and management of spine injuries.
Frequently Asked Questions
What Are the Potential Risks and Side Effects of These Diagnostic Procedures?
Diagnostic procedures bear potential risks such as infection, radiation exposure, and allergic reactions. Side effects may include discomfort and bleeding. Procedure costs can be high, but diagnostic innovations are working to improve safety and affordability.
How Accurate Are These Diagnostic Techniques in Identifying Specific Spine Injuries?
Diagnostic techniques for spinal injuries, despite their limitations, are generally accurate. Injury severity often dictates the technique used. Advanced imaging like MRI and CT scans provide detailed views, enabling precise identification of specific spinal injuries.
How Long Does It Typically Take to Receive Results From These Diagnostic Tests?
The duration for receiving results from diagnostic tests varies, often depending on the test utilized. With proper patient preparation and management of test anxiety, results can typically be obtained within a few days to a week.
What Happens if a Spine Injury Is Not Detected in the Initial Stages?
If a spine injury is not detected during the initial stages, long term consequences can ensue. These can include chronic pain, reduced mobility, or neurological issues, often exacerbated by the delayed identification of initial symptoms.
Are There Any Alternative Methods for Diagnosing Spine Injuries if I Cant Undergo Traditional Techniques?
Yes, alternative methods for diagnosing spine injuries include MRI, CT scans, and nerve conduction studies. However, these may involve higher diagnosis costs and varied patient experiences compared to traditional radiographic techniques.